A game-changer for stroke treatment
Stroke is the leading cause of severe long-term disability in the United States, and less than 40 percent of patients who experience the most severe form of stroke regain functional independence if they receive the standard drug intervention alone. Now a study by an international group of stroke physician-researchers has found that removal of the clot causing a severe stroke, in combination with the standard medication, improves the restoration of blood flow to the brain and may result in better long term outcomes.
The findings of the Swift Prime trial (Solitaire With the Intention For Thrombectomy as PRIMary Endovascular treatment) were reported April 17 in the online edition of the New England Journal of Medicine and are scheduled to be published in the journal’s June 11 print edition.
“These findings are a game-changer for how we should treat certain types of stroke,” says Dr. Demetrius Lopes, surgical director of the comprehensive stroke center at Rush University Medical Center and a co-author of the study. “These outcomes are the difference between patients being able to care for themselves after stroke and being dependent.”
Rush was one of the 39 centers in the U.S. and Europe that participated in the Swift Prime trial.
Out, Damned Clot!
More than 795,000 people have a stroke each year, according to the U.S. Centers for Disease Control and Prevention. About 87 percent of these incidents are ischemic strokes, which result from clots in vessels supplying blood to the brain.
The standard treatment for ischemic stroke within the first three to four and a half hours of symptoms is intravenous tissue plasminogen activator (IV tPA), a medication which dissolves the clot. However in the approximately 20 percent of cases in which one of the major arteries is blocked, resulting in a severe stroke, IV tPA alone may not be sufficient to dissolve the clot. If a patient experiencing a severe stroke is brought to a qualified hospital in time, doctors also may be able to perform a minimally invasive procedure called thrombectomy to remove the clot.
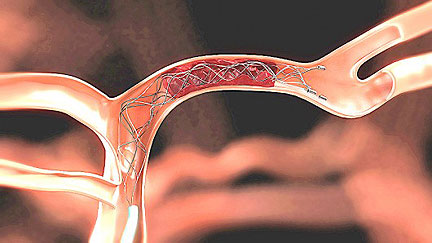 During thrombectomy, a neurovascular surgeon threads a catheter through an incision in the patient’s groin, snaking it through the blood vessels and into the brain. The doctor then uses a device attached to the catheter to grab and dislodge the clot and pull it all the way out through the incision, a bit like an angler reeling in a fish.
During thrombectomy, a neurovascular surgeon threads a catheter through an incision in the patient’s groin, snaking it through the blood vessels and into the brain. The doctor then uses a device attached to the catheter to grab and dislodge the clot and pull it all the way out through the incision, a bit like an angler reeling in a fish.
One More Out of Every Four
The Swift Prime study randomly divided patients with severe ischemic strokes into two groups, one receiving IV tPA alone, and the other receiving combination therapy of IV tPA and thrombectomy within six hours of the onset of stroke symptoms. (IV tPA currently is the only treatment for ischemic stroke approved by the U.S. Food and Drug Administration, but the use of thrombectomy is allowed in clinical trials.)
In all, 196 patients - 98 in each group - at 39 centers in the U.S. and Canada participated in the study between December 2012 and November 2014.
The researchers assessed each patient’s level of disability after 90 days using a standardized measurement. The study found that the patients who received IV tPA plus thrombectomy exhibited reduced disability across the entire range of the measurement, with a functional independence rate of 60 percent compared to 35.5 percent for those patients who received only IV tPA.
“For every 2.6 patients treated, one additional patient had an improved disability outcome; for every four patients treated, one additional patient was independent at 90 day follow-up,” the New England Journal of Medicine article declares.
The study also found that patients who received thrombectomy had better cerebral blood flow rates: At 27 hours after treatment, 82.8 percent of those patients had blood flow that was 90 percent of normal or better, versus 40.4 percent of patients who only received IV tPA.
The study’s findings depart from three previous trials that did not find thrombectomy provided greater benefits than IV tPA alone. “The Swift Prime trial used better technology, better imaging and quicker intervention, and we obtained a different result,” Lopes says.
In fact, Swift Prime was one of four recent worldwide studies that evaluated newer thombectomy devices and techniques. The result of the first study, reported in the New England Journal of Medicine in December, found such strong evidence of the benefit of thrombectomy that the other trials were halted.
“Ethically, we can’t deny patients a treatment when we have such strong evidence it’s better for them,” Lopes says. At Rush and other study locations, thrombectomy now is a standard treatment within the first few hours for patients with severe strokes.
“Time Equals Brain”
However, time remains crucial in stroke treatment. For every minute that a stroke is untreated, a patient loses 1.9 million brain cells and 14 billion connections between brain cells - a phenomenon underlying the stroke awareness adage “time equals brain.”
“The majority of the positive results of these trials were found in patients treated within four hours, six hours tops,” observes Dr. James Conners, medical director of the Rush comprehensive stroke center.
Of all the participating sites in the Swift Prime trial, Rush was found to provide the fastest times from patient arrival to insertion of the catheter and from initiation of the procedure to restoration of blood flow, both of which are critically important to improving patient’s outcomes.
The Rush stroke team also was recognized for having the best workflow among a larger group of 203 sites in the U.S., Europe, Canada and Australia that participated in Swift Prime and two other affiliated stroke studies. Workflow refers to the coordination of the stroke team - including emergency medicine personnel, neurologists, neurosurgeons and neurointensive care specialists - to provide quick treatment.
Time for a Change
Lopes and Conners believe the results of these studies demonstrate the need for a different approach to stroke care. Conners notes that nationwide, the average usage of IV tPA in U.S. stroke cases is only about five percent. “It’s far below where we need to be,” he says.
He believes that educating people to recognize signs of stroke and call 911, and taking steps to make sure they’re taken to the right facility, would improve usage to 50 percent. “We’re constantly working with the city’s Emergency Medical Services division and the emergency department at Rush to get the stroke recognized and treated as soon as possible,” Conners says.
Lopes points out that Rush currently is one of only a few hospitals in Chicago that can perform thrombectomy. “Many of the stroke patients who could benefit from it can’t be brought here in time,” he says. “We need to make the treatment standard.”
In addition, Lopes feels that paramedics need additional training and equipment that would enable them to screen stroke patients in the field and determine which ones would benefit from thrombectomy.
“Rush is doing great from getting our patients from the door of the hospital to fixing the problem,” he says. “We can do even better as a city if we can get patients who need thrombectomy even faster to the hospitals that can provide that care.”
###
Kevin McKeough
.(JavaScript must be enabled to view this email address)
312-942-7820
Rush University Medical Center
Journal
New England Journal of Medicine