Probiotics linked to lower risk of allergies for kids
Babies whose mothers take probiotics while pregnant and those who are given the so-called “good bacteria” supplements early in life may be at lower risk for allergies but not asthma than other kids, according to a new analysis of past studies.
Doctors don’t typically recommend for or against probiotics for pregnant women or young children, and it’s still too soon to make that leap, said senior author Dr. Erick Forno of Children’s Hospital of Pittsburgh.
“Based on our findings, probiotics have a protective effect against allergies, but we still have things to learn before we can give general advice to the public,” he told Reuters Health in an email.
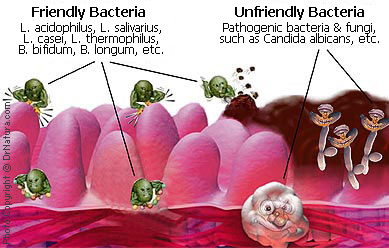
Bacteria living in the gut and digestive tract have been linked to immune system health. So getting enough probiotics - microorganisms like those in yogurt and yeast that have a beneficial effect on the balance of gut microbes - might logically help support a healthy immune system as well, researchers said.
Since allergies and asthma both spring from hypersensitive immune responses, several trials have set out to assess the effect of probiotic supplements on those conditions.
Trials most often use probiotic supplements in pill form because dosing is easier to control, but there is no reason to believe dietary probiotics like those in yogurt wouldn’t also be effective, Forno said.
 His team analyzed the results of 25 trials of supplements given during pregnancy or within the first year of a child’s life. All of the studies compared mothers and babies randomly assigned to take probiotics with those given placebo supplements.
His team analyzed the results of 25 trials of supplements given during pregnancy or within the first year of a child’s life. All of the studies compared mothers and babies randomly assigned to take probiotics with those given placebo supplements.
Participants were given probiotic doses daily, and in some cases more than daily, for a few months to a year.
The trials tracked whether kids went on to test positive for common allergies - such as peanut or pollen allergies - and whether they wheezed or showed signs of asthma, based on a questionnaire given to parents.
Babies who were exposed to probiotics in the womb and received supplements after birth had a 12 percent lower risk of allergies in the following months and years than kids in the comparison groups. But allergy risk was not reduced when babies were started on probiotics after birth only.
 Postnatal probiotics may not be necessary to see a beneficial effect, but further studies would be needed to clarify that point, according to Mimi Tang, director of the department of allergy and immunology at Royal Children’s Hospital in Parkville, Australia.
Postnatal probiotics may not be necessary to see a beneficial effect, but further studies would be needed to clarify that point, according to Mimi Tang, director of the department of allergy and immunology at Royal Children’s Hospital in Parkville, Australia.
There did not seem to be a difference in asthma risk for kids who received probiotics, the researchers reported in Pediatrics.
“It must be noted though that only a few of the studies followed subjects beyond age five and diagnosis of asthma is not clear under this age, so most of the studies are really only reporting on wheezing episodes which may not necessarily be asthma,” Tang, who was not involved in the review, told Reuters Health.
Probiotics are generally regarded as safe and studies have not found serious side effects, but it’s still not clear which specific microbes are best and at what dosage, she said.
Forno said the new findings may help bolster the so-called hygiene hypothesis.
“As nations have become more industrialized and developed, they have also become cleaner, and therefore our exposure to microbes early in life has decreased, and this has decreased infections,” he said.
The hygiene hypothesis posits that the cleaner environment may have led to an increase in allergies and asthma.
“The theory is that such exposures in early life helped our immune system to learn how to ‘self regulate’ and recognize what to fight and what not to,” he said.
“Our hope is that with the results from our study, researchers will move on from trying to determine ‘if’ probiotics help prevent allergies, and into ‘how’ or what the best approach may be.”
SOURCE: Pediatrics, online August 19, 2013
###
Probiotic Administration in Early Life, Atopy, and Asthma: A Meta-analysis of Clinical Trials
RESULTS: Probiotics were effective in reducing total immunoglobulin E (IgE) (mean reduction: –7.59 U/mL [95% confidence interval (CI): –14.96 to –0.22]; P = .044). Meta-regression showed that the reduction in IgE was more pronounced with longer follow-up. Probiotics significantly reduced the risk of atopic sensitization when administered prenatally (relative risk: 0.88 [95% CI: 0.78 to 0.99]; P = .035 for positive result on the skin prick test and/or elevated specific IgE to common allergens) and postnatally (relative risk: 0.86 [95% CI: 0.75 to 0.98]; P = .027 for positive result on skin prick test). Administration of Lactobacillus acidophilus, compared with other strains, was associated with an increased risk of atopic sensitization (P = .002). Probiotics did not significantly reduce asthma/wheeze (relative risk: 0.96 [95% CI: 0.85 to 1.07]).
CONCLUSIONS: Prenatal and/or early-life probiotic administration reduces the risk of atopic sensitization and decreases the total IgE level in children but may not reduce the risk of asthma/wheeze. Follow-up duration and strain significantly modified these effects. Future trials for asthma prevention should carefully select probiotic strain and consider longer follow-up.
Nancy Elazab, MD,
Angelico Mendy, MD, MPH,
Janvier Gasana, MD, PhD,
Edgar R. Vieira, PhD,
Annabelle Quizon, MD, and
Erick Forno, MD, MPH