Opioids for chronic pain: Study looks at how patients and their doctors talk about risks
Although the popular press - from entertainment news to the crime blotter - has paid significant attention to the dangers of hydrocodone, oxycodone and other opioids, little is known about whether and how this issue comes up in discussions between chronic pain patients and their physicians.
A pilot study by researchers from the Roudebush VA Medical Center and the Regenstrief Institute is believed to be the first to analyze the nature of these conversations in regular primary care appointments. A better understanding of how patients and doctors discuss these potentially addictive pain medications may ultimately lead to more effective strategies for communicating about chronic pain treatment.
‘’‘I’m Not Abusing or Anything’: Patient-physician communication about opioid treatment in chronic pain” is published in the November issue of Patient Education and Counseling, the official journal of the American Academy on Communication in Healthcare and of the European Association for Communication in Healthcare.
The study followed 30 patients with chronic pain. They were audio-recorded during visits with their primary care doctor and then interviewed about their pain care as well as their relationship with their physicians.
“Chronic pain - pain lasting more than six months - is a debilitating problem for many individuals,” said study first author Regenstrief Institute investigator Marianne S. Matthias, Ph.D., a VA research scientist and an adjunct assistant professor of communication studies in the School of Liberal Arts at Indiana University-Purdue University Indianapolis. “Although it is well established that opioid treatment for chronic pain poses numerous uncertainties, little has been reported in previous studies about how patients and their physicians actually discuss these uncertainties in clinic appointments.
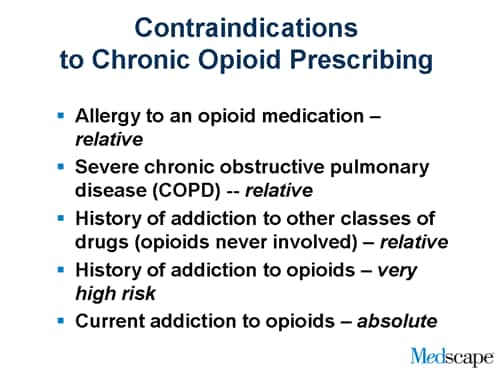
 “Our study provides a window into how uncertainty about potential addiction and misuse of opioids is managed through patient-physician communication. We heard candid discussions revealing concern by both patients and their physicians about a range of issues including past alcoholism and past marijuana or cocaine use.
“Our study provides a window into how uncertainty about potential addiction and misuse of opioids is managed through patient-physician communication. We heard candid discussions revealing concern by both patients and their physicians about a range of issues including past alcoholism and past marijuana or cocaine use.
“There is an important message here for people with chronic pain and for the doctors who treat them. If patients and their doctors have a relationship marked by mutual trust and a strong therapeutic alliance, they are better positioned to candidly discuss all chronic pain treatment options, including risks and benefits of opioid treatment, with the ultimate goal being to develop the most appropriate and effective treatment plan for each individual patient.” said Dr. Matthias, a health services researcher and communication scientist.
Three patterns of physician responses to uncertainty about prescribing opioids were observed in the audio-recordings: reassurance, avoiding opioids and gathering additional information.
###
 In addition to Dr. Matthias, co-authors of the study are former Regenstrief Institute investigator Erin E. Krebs, M.D., M.P.H., now with the Minneapolis VA and the University of Minnesota; Linda A. Collins, B.S., and Jessica Coffing, MPH, of the Roudebush VA; former Regenstrief Institute fellow Alicia A. Bergman, now with the Los Angeles VA; and Regenstrief Institute investigator Matthew J. Bair, M.D., M.S., a VA research scientist and associate professor of medicine at Indiana University School of Medicine. Dr. Bair is an internist specializing in pain management.
In addition to Dr. Matthias, co-authors of the study are former Regenstrief Institute investigator Erin E. Krebs, M.D., M.P.H., now with the Minneapolis VA and the University of Minnesota; Linda A. Collins, B.S., and Jessica Coffing, MPH, of the Roudebush VA; former Regenstrief Institute fellow Alicia A. Bergman, now with the Los Angeles VA; and Regenstrief Institute investigator Matthew J. Bair, M.D., M.S., a VA research scientist and associate professor of medicine at Indiana University School of Medicine. Dr. Bair is an internist specializing in pain management.
This work was supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development (CDA 10-034) and a Young Investigator Award from the Indiana Institute for Medical Research. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the United States government.
###
Cindy Fox Aisen
.(JavaScript must be enabled to view this email address)
317-843-2276
Indiana University