Current practice may over-diagnose vitamin D deficiency
The current “gold standard” test for measuring vitamin D status may not accurately diagnose vitamin D deficiency in black individuals. In an article in the Nov. 21 New England Journal of Medicine, a team of researchers report finding that genetic differences in a vitamin D carrier protein referred to as D-binding protein may explain the discrepancy between the prevalence of diagnosed vitamin D deficiency in black Americans - based on measuring the molecule 25-hydroxyvitamin D (25OHD) - and a lack of the usual symptoms of vitamin deficiency.
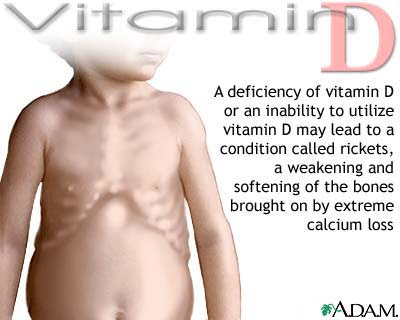
The essential role of vitamin D in maintaining bone health is well recognized, but while measurement of 25OHD alone consistently classifies from 70 to 90 percent of black Americans as vitamin D deficient, the usual consequences of deficiency - such as low bone density and increased fracture risk - are actually less prevalent among black individuals. That inconsistency led the team led by Ravi Thadhani, MD, MPH, chief of the Division of Nephrology in the Massachusetts General Hospital (MGH) Department of Medicine, to take a closer look at whether current methods accurately determine vitamin D deficiency.
The investigators examined data from more than 2,000 participants in HANDLS (Healthy Aging in Neighborhoods of Diversity Across the Life Span), a larger National Institutes of Health (NIH)-sponsored study, led by Michele K. Evans, MD, co-corresponding author of the current report, and Alan B. Zonderman, PhD, also a co-author. HANDLS is prospective, long-term, epidemiologic study of age–associated health disparities in socioeconomically diverse black and white individuals in the city of Baltimore. Participants - adults ages 30 to 64 - were interviewed and received medical examinations between 2004 and 2009.
For the current study, researchers analyzed levels of 25OHD, levels and genetic variants of D-binding protein, and levels of calcium and parathyroid hormone - another marker of vitamin D deficiency - along with bone density readings in almost 1,200 white and around 900 black participants.
The results indicated that black participants had significantly lower levels of both 25OHD and D-binding protein, compared with white participants and also showed that about 80 percent of the difference in D-binding protein levels could be explained by genetic variation. However, bone density and calcium levels were higher in black participants, and while their parathyroid hormone levels also were higher, the difference between black and white participants was slight.
“Black people are frequently treated for vitamin D deficiency, but we may not be measuring the right form of vitamin D to make that diagnosis,” says Thadhani, who is senior and co-corresponding author of the NEJM report. “While our finding that 80 percent of black participants in this study met criteria for vitamin D deficiency is consistent with previous studies, we were surprised to find no evidence of problems with bone health. Most vitamin D in the bloodstream is tightly bound to D-binding protein and is not active. When we determined the concentrations of circulating non-bound vitamin D, which would be available to cells, we found that levels of this form were equivalent between black and white participants, which suggested to us that these black individuals may not be truly deficient.”
 He adds, “Although currently there are no commercially available assays that directly measure bioavailable levels of 25OHD, these results suggest that such assays would more accurately identify those with true vitamin D deficiency, allowing us to direct treatment toward those who really need it. Additional studies need to be conducted to establish optimal levels of bioavailable 25ODH across all racial and ethnic groups.” Thadhani is a professor of Medicine at Harvard Medical School.
He adds, “Although currently there are no commercially available assays that directly measure bioavailable levels of 25OHD, these results suggest that such assays would more accurately identify those with true vitamin D deficiency, allowing us to direct treatment toward those who really need it. Additional studies need to be conducted to establish optimal levels of bioavailable 25ODH across all racial and ethnic groups.” Thadhani is a professor of Medicine at Harvard Medical School.
Evans, who is deputy scientific director and chief of the Health Disparities Research Section at the National Institute on Aging Intramural Research Program (NIA-IRP), notes, “This study confirms the value of addressing clinical questions from a health disparities standpoint that overcomes barriers to inclusion of diverse populations in biomedical research.”
###
Camille Powe, M.D., of Brigham and Women’s Hospital is lead author of the NEJM. Additional co-authors are Julia Wenger, MPH, Hector Tamez, MD, MPH, and Ishir Bhan, MD, MPH, MGH Nephrology; Michael Nalls, PhD, NIA-IRP; Anders Berg, MD, PhD, Dongsheng Zhang, PhD, and Ananth Karumanchi, MD, Beth Israel Deaconess Medical Center; and Neil Powe, MD, University of California, San Francisco. The study was supported by National Institute of Aging grant AG000513 and National Institutes of Health grants K24 DK094872 and R01 DK094486.
Massachusetts General Hospital, founded in 1811, is the original and largest teaching hospital of Harvard Medical School. The MGH conducts the largest hospital-based research program in the United States, with an annual research budget of more than $775 million and major research centers in AIDS, cardiovascular research, cancer, computational and integrative biology, cutaneous biology, human genetics, medical imaging, neurodegenerative disorders, regenerative medicine, reproductive biology, systems biology, transplantation biology and photomedicine.
###
Cassandra Aviles
.(JavaScript must be enabled to view this email address)
617-724-6433
Massachusetts General Hospital