A new study indicates that there is no apparent benefit to arthroscopic knee surgery for age-related tears of the meniscus in comparison with nonsurgical or sham treatments. The study, published in CMAJ (Canadian Medical Association Journal), provides evidence that middle-aged or older patients with mild or no osteoarthritis of the knee may not benefit from the procedure.
As people age, the meniscus in the knee thins and becomes less flexible and more susceptible to tearing. When the meniscus tears, it can cause pain and mechanical symptoms. Arthroscopic knee surgery (meniscal débridement) is one of the most common orthopedic surgical procedures, with more than 4 million performed each year around the world. This surgical technique is commonly used to address degenerative meniscus tears. The procedure involves making small (keyhole-type) incisions to remove the torn fragments from the damaged meniscus. Although the surgery is minimally invasive, there may still be complications; these risks must be weighed against benefits to the patient.
Two previous studies showed that for patients with severe knee arthritis, arthroscopic knee surgery is not effective for long-term symptom relief.
To determine whether arthroscopic knee surgery for degenerative meniscal tears would provide relief to patients with mild or no osteoarthritis, researchers analyzed seven randomized controlled trials.
The sample total was 811 knees in 805 patients with a mean age of 56 years. In four trials, there was no short-term pain relief in the first six months after surgery for patients with some osteoarthritis, nor was there improvement in long-term function up to two years later in five trials.
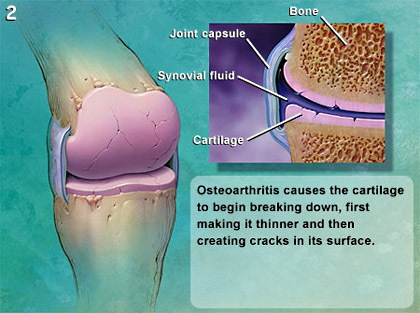
What happens to a knee with osteoarthritis?
When your knee has osteoarthritis its surfaces become damaged and it doesn’t move as well as it should do. The following happens:
- The cartilage becomes rough and thin - this can happen over the main surface of your knee joint and in the cartilage underneath your kneecap.
- The bone underneath the cartilage reacts by growing thicker and becoming broader.
- All the tissues in your joint become more active than normal, as if your body is trying to repair the damage.
- The bone at the edge of your joint grows outwards, forming bony spurs called osteophytes.
- The synovium may swell and produce extra fluid, causing the joint to swell - this is called an effusion or sometimes water on the knee.
- The capsule and ligaments slowly thicken and contract.
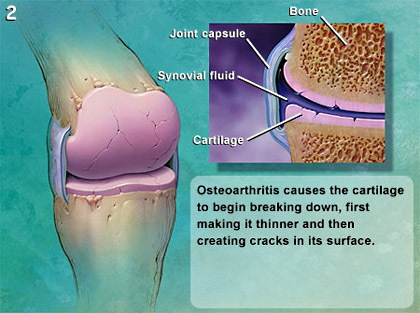 These changes in and around your joint are partly the result of the inflammatory process and partly an attempt by your body to repair the damage. In many cases your body’s repairs are quite successful and the changes inside your joint won’t cause much pain or, if there is pain, it’ll be mild and may come and go.
These changes in and around your joint are partly the result of the inflammatory process and partly an attempt by your body to repair the damage. In many cases your body’s repairs are quite successful and the changes inside your joint won’t cause much pain or, if there is pain, it’ll be mild and may come and go.
However, in other cases the repair doesn’t work as well and your knee is damaged. This leads to instability and more weight being put onto other parts of the joint. This can cause symptoms to become gradually worse and more persistent over time.
“Arthroscopic surgery for degenerative meniscal tears in the setting of mild or no concurrent osteoarthritis in middle-aged patients may have little, if any, effect on short-term (< 6 mo) and long-term (< 2 yr) outcomes in comparison with nonoperative management," writes Dr. Moin Khan, Division of Orthopedic Surgery, Department of Surgery, McMaster University, Hamilton, Ontario, with coauthors.
Physicians need to carefully weigh the costs and benefits when deciding which middle aged patients should undergo surgery. "With limited evidence supporting arthroscopic meniscal débridement for degenerative meniscus tears in the setting of mild or no concomitant osteoarthritis, an initial trial of nonoperative interventions should play a large role for middle-aged people."
Expert Q&A:
When should I start considering some form of knee replacement surgery?
The general rule is when the pain becomes continuous, is unresponsive to other conservative measures, and is interfering significantly with daily living and your quality of life. If you have pain at rest or pain at night, that’s one strong indication that it’s time for a replacement. You can’t go just by an X-ray, though. Some people’s X-rays look terrible, but their pain level and functioning is adequate.
Is age a factor when it comes to knee replacements?
Paradoxically, the younger and more active you are, the less likely you are to be satisfied with a knee replacement. Younger patients have higher expectations. In general, the elderly aren’t concerned about playing tennis; they just want pain relief and to be able to get around. It’s easier for the elderly in other ways as well. Elderly people don’t feel as much pain in recovery. Also, the older you are, the more likely your knee will last for your lifetime. An active 40-year-old will probably need another one eventually.
What kinds of activities will I be able to do after a knee replacement? Will I still have pain after getting back to normal activity levels?
You can walk all you want, golf, play sports like non-aggressive doubles tennis—but no diving for balls or running all over the court. I discourage high-impact sports that involve twisting or turning, like skiing or basketball. An avid gardener will have a difficult time because it’s hard to kneel with a knee replacement. Keep in mind that the less stress you put on your knee, the longer it will last.
How do you select a surgeon?
Ask the surgeon how many knees he does per year. He should do a couple of hundred. His infection rate should be under one percent. Ask about his general outcomes, and whether or not he tracks outcomes, including range of motion and loosening rate. Statements like “our patients do great,” aren’t good enough.
I’ve heard about minimally invasive knee surgery. Am I a candidate for that?
Minimally invasive is a misnomer. No matter how small the incision, you still have to drill and cut the bone. There’s no advantage to a smaller incision, but there are disadvantages, such as it takes longer, and there’s an increased risk to bone or arteries. The durability of the device is decreased because you can’t put it in as well, and you can’t use devices with longer components. Also, it can only be done with thin people. There’s no difference in the amount of bleeding or recovery time. Even the incision is only an inch shorter. It’s simply not worth it
How about arthroscopic knee surgery, where they clean out the joint. Should I try that first?
The Journal of the American Medical Association recently published an article stating there is zero benefit to it. It’s no better than cortisone injections, and it’s a lot more invasive.
###
orthopedic surgeon Dr. Henry A. Finn, M.D., F.A.C.S., Medical Director of the University of Chicago Bone and Joint Replacement Center at Weiss Hospital
###
Kim Barnhardt
.(JavaScript must be enabled to view this email address)
613-520-7116 x2224
Canadian Medical Association Journal
Provided by ArmMed Media
 These changes in and around your joint are partly the result of the inflammatory process and partly an attempt by your body to repair the damage. In many cases your body’s repairs are quite successful and the changes inside your joint won’t cause much pain or, if there is pain, it’ll be mild and may come and go.
These changes in and around your joint are partly the result of the inflammatory process and partly an attempt by your body to repair the damage. In many cases your body’s repairs are quite successful and the changes inside your joint won’t cause much pain or, if there is pain, it’ll be mild and may come and go.