Anti-epilepsy drug preserves brain function after stroke
New research suggests that an already-approved drug could dramatically reduce the debilitating impact of strokes, which affect nearly a million Americans every year.
In the study, one dose of the anti-epilepsy drug, retigabine, preserved brain tissue in a mouse model of stroke and prevented the loss of balance control and motor coordination. Researchers from the School of Medicine at The University of Texas Health Science Center at San Antonio conducted the study, which was published Feb. 3 in The Journal of Neuroscience.
Balance and coordination test
Hours after a stroke, both treated mice and a control group of mice were placed on a balance beam to observe motor coordination. The untreated mice displayed a pronounced loss of coordination with slips and falls. Treated mice had no difficulty with balance, ambulation or turning around on the beam.
“You couldn’t even tell they had a stroke,” said senior author Mark S. Shapiro, Ph.D., professor of physiology at the UT Health Science Center San Antonio. “They ran across the balance beam like gymnasts.”
Histological analysis of the brain tissue of treated mice showed significantly reduced damage to the tissue after the stroke, compared to untreated mice. The protective effects of the medication were observed in treated mice up to five days after the stroke, said Sonya Bierbower, Ph.D., postdoctoral fellow and lead author of the report.
Duration of effect
 Future studies will assess how long brain function can be protected after a stroke, and whether injury-related seizures can be prevented. “We are also going to see if we can prevent strokes in high-risk animal models,” Dr. Bierbower said.
Future studies will assess how long brain function can be protected after a stroke, and whether injury-related seizures can be prevented. “We are also going to see if we can prevent strokes in high-risk animal models,” Dr. Bierbower said.
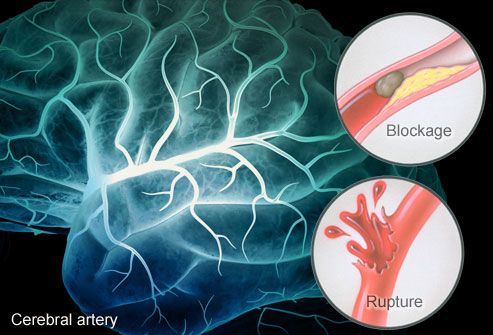
Retigabine and similar agents open specific proteins called potassium ion channels, whose action stops the electrical activity of nerve cells in the brain. The San Antonio team studied ischemic stroke, in which oxygen and nutrients are suddenly cut off due to a clot in a blood vessel. This is the type of stroke most often seen in humans. “We thought if we could stop the neurons from firing, stopping their electrical activity, we could conserve their resources until the time their blood supply was restored,” Dr. Shapiro said. “This proved to be the case.”
Cells starved of oxygen and nutrients for six hours are compromised and the process of dying is nearly impossible to reverse. Moreover, when cells die, they release factors that trigger many types of responses including an inflammatory response, leading to more cell death in the areas around the blood clot.
tPA for clots
A drug called tissue plasminogen activator (tPA) treats stroke by dissolving clots to restore blood flow, but this has significant limitations. tPA causes severe thinning of the blood, so it is not an option for patients who have high blood pressure, a history of bleeding or weak blood vessels. tPA is most effective in the first hours after a stroke, but its later use may do more damage than good.
Directly affecting nerve cells
Potassium channel openers such as retigabine work on a completely different system. “They have nothing to do with thinning blood, but preserving cells by putting a brake on their electrical activity,” Dr. Shapiro said.
“It’s treating the first step in the sequence and stopping the more damaging secondary effects,” Dr. Bierbower said. “These agents directly affect the nerve cells themselves.”
FDA approved for epilepsy
Because retigabine is approved by the U.S. Food and Drug Administration under the American brand name Ezogabine as an anticonvulsant, physicians may use it off label in stroke patients. FDA approval for specifically this drug as stroke therapy will require a clinical trial to be conducted, and a team of neurologists and neurosurgeons at the Health Science Center is considering it, Dr. Shapiro said.
“As a leading cause of death and disability, stroke poses a major risk to our society,” said David F. Jimenez, M.D., FACS, professor and chairman of the Department of Neurosurgery at the Health Science Center. “It is very exciting to see that our collaborative work with our colleagues in physiology could provide a superb way to ameliorate the harmful effects of stroke on our patients.”
###
Acknowledgments
Drs. Bierbower and Shapiro both received funding from the National Institute of Neurological Disorders and Stroke to conduct this study. A grant from the American Heart Association has been applied for to further this work. James D. Lechleiter, Ph.D., professor of cellular and structural biology in the School of Medicine, is a co-author of the study.
For current news from the UT Health Science Center San Antonio, please visit our news release website, like us on Facebook or follow us on Twitter.
The University of Texas Health Science Center at San Antonio, one of the country’s leading health sciences universities, ranks in the top 13 percent of academic institutions receiving National Institutes of Health (NIH) funding. The university’s schools of medicine, nursing, dentistry, health professions and graduate biomedical sciences have produced more than 31,000 graduates. The $787.7 million operating budget supports eight campuses in San Antonio, Laredo, Harlingen and Edinburg.
###
Will Sansom
.(JavaScript must be enabled to view this email address)
210-567-2579
###
University of Texas Health Science Center at San Antonio
Journal
Journal of Neuroscience