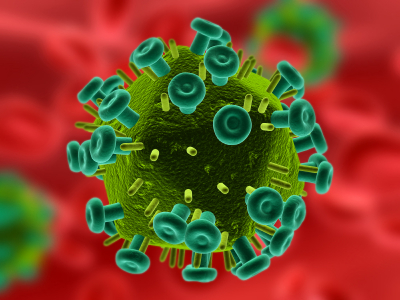
HIV virus spread and evolution studied through computer modeling
Researchers at Los Alamos National Laboratory are investigating the complex relationships between the spread of the HIV virus in a population (epidemiology) and the actual, rapid evolution of the virus (phylogenetics) within each patient’s body.
“We have developed novel ways of estimating epidemics dynamics such as who infected whom, and the true population incidence of infection versus mere diagnoses dates,” said Thomas Leitner, principal investigator. “Obviously, knowledge about these things is important for public health monitoring, decision making and intervention campaigns, and further to forensic investigations.”
The team models the uninfected population using traditional differential equations on the computer; this is done for computational speed, because an agent-based component is much more demanding. Once a person is infected, he/she becomes an “agent” in computer modeling terms, and the model starts following their behavior individually, as well as the viral HIV evolution within the person.
Agent-based modeling clarifies infection history
This new modeling approach distinguishes between susceptible and infected individuals to capture the full infection history, including contact tracing data for infected individuals. The uninfected individuals are modeled at a population level and stratified by transmission risk and social group. The social network in this model forms - and can change - during the simulation. Thus, the model is much more realistic than traditional models.
The advantage of this epidemiological model, Leitner said, is that “it allows us to simulate many possible outcomes of epidemics with known parameters of human interactions, where social networks form as part of the agent interactions. It is a flexible system that has the ability to describe realistic human populations.”
 Within a National Institutes of Health-supported project “Reconstructing HIV Epidemics from HIV Phylogenetics,” the team has published 10 papers describing new mathematical models and results from real data addressing these issues. Most recently, they published a Nature correspondence on the limitations of HIV forensics and the need for better standards.
Within a National Institutes of Health-supported project “Reconstructing HIV Epidemics from HIV Phylogenetics,” the team has published 10 papers describing new mathematical models and results from real data addressing these issues. Most recently, they published a Nature correspondence on the limitations of HIV forensics and the need for better standards.
Who infected whom
A key question is on the fundamental limitations to the inference of who infected whom, based on a concept known as the pre-transmission interval (which this group first described back in 1999). Another publication, published in Epidemics, developed a new hybrid model to simulate and analyze the spread of HIV or other pathogens spread in a human population. The work also appeared in PLoS-ONE Public Library of Science online publication.
The infection is caused by one of several related retroviruses that become incorporated into host cell DNA and result in a wide range of clinical diseases. These vary from asymptomatic carrier states to severe debilitating diseases that lead ultimately to death.
Two closely related viruses, HIV-1 and HIV-2 have been identified as causing AIDS in different geographic regions. HIV-1 causes most cases of AIDS in the Western Hemisphere. HIV-2 is less virulent and is the principal agent of AIDS in West Africa.
Some forms of HIV may not cause disease at all. Researchers are following a group of patients in Australia, so-called “nonprogressors” who have been infected with a single strain of HIV for more than 12 years with no sign of AIDS.
MOLECULAR BIOLOGY AND THE ORIGIN OF HIV
As the technology of analyzing genetic material improved during the 1980s it became possible to compare all of the various monkey and human HIV viruses nucleotide by nucleotide, noting where similarities and differences existed. Using such techniques, scientists would begin to construct family trees for the viruses. They were doing lineages of evolution that resemble those used by paleoanthropologists who study evolution.
At the heart of the technique, which is called molecular epidemiology were a few key assumptions: the more alike two viral genetic were, the more likely it was that they shared a common and recent ancestor. This is like Darwin’s finches on the Galapagos Islands. With them, Darwin had concluded, the similarity implied a common finch ancestor.
Like human evolution, viral evolution takes time. The degrees of viral variation could be correlated with a timetable of years or centuries. If you are following this—it is similar to the ‘Eve hypothesis’ discussed in human evolution.
There are certain genetic features that were so essential to the survival of HIVs and SIVs (simian immune virus, the ‘monkey version’ of HIV) that they would be conserved over generations of viruses.
The essential conclusion (you are following this, aren’t you?) Was that is was UNLIKELY that human virus had evolved into monkey virus. The family tree had to have begun with SIV. Each of these assumptions would be challenged in time, but the basic approach would survive criticism.
How close are human and monkey viruses? SIV and HIV were close, sharing more than 75% homology (similarity). HIV-1 had only a 40% homology with either virus. Some strains of HIV-2 and SIV were so similar that scientists concluded that monkey to human transmission had occurred since World War II.
There is one notable exception to the pattern of HIV distribution in human beings: Pygmies. For millennia the Pygmy people had lived in the dense rain forests of Cameroon, Congo, and the Central African Republic, surviving as the continent’s most expert jungle hunters. Monkey meat had always been a part of the Pygmy diet, and the people (particularly male hunters) had frequent and often violent contact with the monkey populations.
You would expect Pygmies to have been exposed to monkey SIV. Such SIV infections have occurred amongst handlers of monkeys who were scratched, bitten, or had needle sticks here in the United States. Blood tests of Pygmy volunteers revealed no cases of HIV-2 or HIV-1 infection. Here is a reminder in case you have forgotten: HIV-2 is the one prevalent in Africa; HIV-1 is here in the United States.
HIV-1 has become such a genetically specialized human killer that scientists were at pains to find ways to infect laboratory monkeys and apes with it. They could not produce clear-cut AIDS in any nonhuman primate. Natural carries (monkeys in Africa) of the various SIVs that they harbored were unharmed by those viruses.
When viral strains collected in a given geographic location over a period of years were compared, the GenBank study group found that HIV-1 was evolving (mutating) at an overall rate of 1 percent a year. This is astonishing when you consider that mitochondrial DNA used in the Eve hypothesis studies mutates at only 2-4% every million years! Nuclear DNA mutates much more slowly.
Studies of the mutation of HIV-1 suggests that some change took place in the disease epidemiology about 1975 in Central Africa. Scientists refer to this as the ‘big bank’ theory in HIV origins. Not everyone endorses this idea.
As an example, the team modeled a Latvian HIV-1 epidemic, and they showed that injecting drug users fueled the heterosexual population, thereby sustaining the overall epidemic. The researchers are now expanding this hybrid model to also include HIV genetic evolution, which occurs in every infected individual.
The researchers have shown that in fast HIV epidemics - such as among individuals injecting themselves with drugs – HIV viral evolution is slow, resulting in little diversification at the population level. Meanwhile, slower-spreading epidemics display more HIV evolution over the same amount of time.
New field of phylodynamics evolves
 Understanding HIV’s genetic evolution will soon allow investigations of how accurately researchers can reconstruct different epidemiological scenarios using pathogen genetic materials, an important and growing field called phylodynamics.
Understanding HIV’s genetic evolution will soon allow investigations of how accurately researchers can reconstruct different epidemiological scenarios using pathogen genetic materials, an important and growing field called phylodynamics.
The team also has developed a new mathematical model that facilitates estimation of when a person was infected with HIV based on a previously used biomarker (BED IgG).
“This is important because most HIV infected persons are not discovered shortly after infection rather, they are often discovered long after, often years after infection, said Leitner. “Thus, to estimate true incidence, that is when infections actually occurred, cannot be done based on diagnosis dates.”
Using Swedish surveillance data, the team has shown that the common assumption that infection occurred on average half way between last negative test and first positive test, is wrong. Instead, the actual infection is strongly skewed towards the first positive sample.
This finding should have large impact on epidemiological models used worldwide by public health organizations, Leitner says. “Currently, we have further developed this model to also correct for unknown cases, such as infected people not yet discovered but who contribute to new infections and thereby the true incidence of the disease.”
The team behind the insights
Researchers include Frederik Graw, Thomas Leitner, Ruy M. Ribeiro, and Helena Skar (Los Alamos National Laboratory) and Jan Albert (Karolinska Institute and Karolinska University Hospital). The National Institutes of Health funded the research.
About Los Alamos National Laboratory
Los Alamos National Laboratory, a multidisciplinary research institution engaged in strategic science on behalf of national security, is operated by Los Alamos National Security, LLC, a team composed of Bechtel National, the University of California, The Babcock & Wilcox Company, and URS for the Department of Energy’s National Nuclear Security Administration.
Los Alamos enhances national security by ensuring the safety and reliability of the U.S. nuclear stockpile, developing technologies to reduce threats from weapons of mass destruction, and solving problems related to energy, environment, infrastructure, health, and global security concerns.
###
Mailing Address
P.O. Box 1663
Los Alamos, NM 87545
Journalist Queries
Communications Office
(505) 667-7000
Los Alamos National Laboratory