Better stent surgery stats needed: heart doctors
But Joynt said doing PCI on these patients may have given them a better chance of survival, even though they ultimately died.
“That’s the kind of overuse (of PCI) that we’re probably willing to accept in many cases,” she said.
However, Joynt’s own research has suggested that hospitals avoid doing PCI in the sickest patients when their states start reporting the number of 30-day deaths.
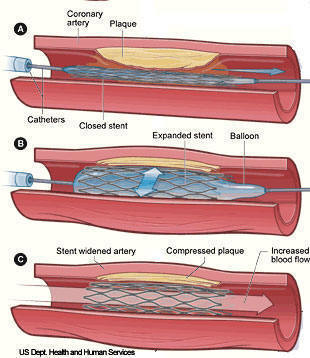
Coronary Angioplasty and Stenting
As a key catheterization-based procedure, coronary balloon angioplasty is used by cardiologists to open blocked coronary arteries. Successful angioplasty can eliminate or delay the need for major coronary bypass surgery. Coronary angioplasty usually goes hand-in-hand with stenting. Balloon angioplasty involves guiding a catheter with a small balloon at its tip into a blocked coronary artery. The balloon is expanded temporarily within the blockage, thus unclogging the artery.
In many cases, the procedure also involves inserting a tiny wire-mesh stent that works as a “scaffold” to keep the blockage propped open. Stents are particularly effective in keeping the artery open for months and years, and thus reducing the incidence of restenosis (renarrowing of the artery). There are currently two types of stents approved by the FDA for use in the United States: bare metal stents (BMS) and drug-eluting stents (DES), the latter of which are coated with drugs to help retard plaque regrowth. Before it is inserted, the stent is mounted (or “crimped”) on the end of a catheter over a deflated balloon. The catheter is moved into the blocked area and the balloon is inflated, deploying the stent permanently against the wall of the artery to keep it open. To prevent blood clots following stenting procedures, anti-clotting drugs including aspirin, clopidogrel and prasugrel are usually prescribed to patients.
Statistics show that balloon angioplasty and stenting procedures have drastically reduced the number of people needing immediate coronary bypass surgery to less than one percent, and to less than 10 percent for those needing such surgery due to restenosis. On the other hand, statistics also reveal that as many as 30 to 50 percent of patients who have had successful balloon angioplasty without stents may experience coronary arterial narrowing once again within six or eight months of their previous angioplasty - in the same area in the artery in which the procedure was performed.
Patients scheduled to undergo coronary balloon angioplasty and stenting procedures may be given medication to prevent blood clots, and will, in most cases, be asked to continue their current medications. No eating or drinking is allowed for at least 12 hours before the procedure. The area of the skin where the catheter enters the body will be numbed by a local anesthetic. The patient will be made drowsy but will not be put to sleep.
Coronary angioplasty and stenting have a success rate greater than 95 percent. However, there are some risks associated with angioplasty or stenting. Plaque (material that builds up on the inner surface) may rebuild in the artery after angioplasty is performed, and bypass surgery may be needed to correct the problem. Angioplasty risks include allergic reaction to the iodine-based contrast, bleeding, damage to the artery requiring emergency surgery, return of the blockage and possible stroke.
Different angioplasty and stent procedures are required for different patients; your physician will discuss the options with you and determine which one best serves your medical needs.
In 2012, her study found that hospitals in Massachusetts, New York and Pennsylvania performed fewer PCIs - especially among the sickest patients who could possibly have benefited the most.
“Public reporting is a good thing and needs to be done, but when done incorrectly there are a lot of downstream consequences, such as denying patients treatment,” said Dr. Duane Pinto, head of interventional cardiology at Boston’s Beth Israel Deaconess Medical Center, who wrote an editorial accompanying the new study.
“We have to recognize and adapt to the unintended consequences of public reporting and fix them when we identify them,” Pinto said.
SOURCE: Journal of the American College of Cardiology, online May 7, 2013
###
Cause of Death Within 30 Days of Percutaneous Coronary Intervention in an Era of Mandatory Outcome Reporting
Results
Of the 4078 PCIs, 81 deaths (2%) occurred within 30 days. Of these, 58% died of cardiac and 42% of non-cardiac causes. However, only 42% of 30-day deaths were attributed to PCI-related complications. Compared to PCI-related, patients with non PCI-related death presented with a higher incidence of cardiogenic shock (15/47 (32%) versus 2/34 (6%); p < 0.01) and cardiac arrest (19/47 (40%) versus 1/34 (3%); p < 0.01). Death certificates had only 58% accuracy (95% CI, 45%-72%) for classifying patients as experiencing cardiac versus non-cardiac death.
Conclusions
Less than half of 30-day deaths are attributed to a PCI-related complication. Death certificates are inaccurate and do not report PCI-related deaths, which may represent a better marker of PCI quality.
Bhuvnesh Aggarwal, MD,
Stephen G. Ellis, MD,
A. Michael Lincoff, MD,
Samir R. Kapadia, MD,
Joseph Cacchione, MD,
Russell E. Raymond, DO,
Leslie Cho, MD,
Christopher Bajzer, MD,
Ravi Nair, MD,
Irving Franco, MD,
Conrad Simpfendorfer, MD,
E. Murat Tuzcu, MD,
Patrick L. Whitlow, MD,
Mehdi H. Shishehbor, DO, MPH