Health Centers > Cancer Health Center > Benign Prostatic Hyperplasia
Benign Prostatic Hyperplasia
Benign Prostatic Hyperplasia Incidence & Epidemiology
BPH is the most common benign tumor in men, and its incidence is age-related. The prevalence of histologic BPH in autopsy studies rises from approximately 20% in men aged 41-50, to 50% in men aged 51-60, and to over 90% in men older than 80. Although clinical evidence of disease occurs less commonly, symptoms of prostatic obstruction are also age-related. At age 55, approximately 25% of men report obstructive voiding symptoms. At age 75, 50% of men complain of a decrease in the force and caliber of their urinary stream.
Risk factors for the development of BPH are poorly understood. Some studies have suggested a genetic predisposition, and some have noted racial differences. Approximately 50% of men under the age of 60 who undergo surgery for BPH may have a heritable form of the disease. This form is most likely an autosomal dominant trait, and first-degree male relatives of such patients carry an increased relative risk of approximately 4-fold.
Benign Prostatic Hyperplasia Etiology
The etiology of BPH is not completely understood, but it seems to be multifactorial and endocrine controlled. The prostate is composed of both stromal and epithelial elements, and each, either alone or in combination, can give rise to hyperplastic nodules and the symptoms associated with BPH. Each element may be targeted in medical management schemes.
Observations and clinical studies in men have clearly demonstrated that BPH is under endocrine control. Castration results in the regression of established BPH and improvement in urinary symptoms. Additional investigations have demonstrated a positive correlation between levels of free testosterone and estrogen and the volume of BPH. The latter may suggest that the association between aging and BPH might result from the increased estrogen levels of aging causing induction of the androgen receptor, which thereby sensitizes the prostate to free testosterone. However, no studies to date have been able to demonstrate elevated estrogen receptor levels in human BPH.
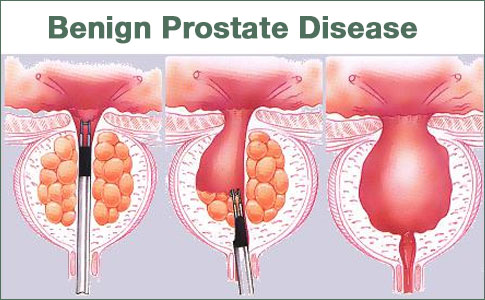
Benign Prostatic Hyperplasia Pathology
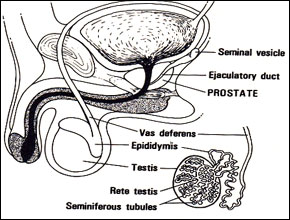
As discussed above, BPH develops in the transition zone. It is truly a hyperplastic process resulting from an increase in cell number. Microscopic evaluation reveals a nodular growth pattern that is composed of varying amounts of stroma and epithelium. Stroma is composed of varying amounts of collagen and smooth muscle. The differential representation of the histologic components of BPH explains, in part, the potential responsiveness to medical therapy. Thus alpha-blocker therapy may result in excellent responses in patients with BPH that has a significant component of smooth muscle, while those with BPH predominantly composed of epithelium might respond better to 5α-reductase inhibitors. Patients with significant components of collagen in the stroma may not respond to either form of medical therapy. Unfortunately, one cannot reliably predict responsiveness to a specific therapy.
As BPH nodules in the transition zone enlarge, they compress the outer zones of the prostate, resulting in the formation of a so-called surgical capsule. This boundary separates the transition zone from the peripheral zone and serves as a cleavage plane for open enucleation of the prostate during open simple prostatectomies performed for BPH.
Benign Prostatic Hyperplasia Pathophysiology
One can relate the symptoms of BPH to either the obstructive component of the prostate or the secondary response of the bladder to the outlet resistance. The obstructive component can be subdivided into the mechanical and the dynamic obstruction.
As prostatic enlargement occurs, mechanical obstruction may result from intrusion into the urethral lumen or bladder neck, leading to a higher bladder outlet resistance. Prior to the zonal classification of the prostate, urologists often referred to the "3 lobes" of the prostate, namely, the median and the two lateral lobes. Prostatic size on digital rectal examination (DRE) correlates poorly with symptoms, in part because the median lobe is not readily palpable.
Benign Prostatic Hyperplasia (BPH)
Incidence & Epidemiology
Etiology
Pathology
Pathophysiology
Clinical Findings
- Symptoms
- Signs
- Laboratory Findings
- Imaging
- Cystoscopy
- Additional Tests
Differential Diagnosis
Treatment
- Watchful Waiting
- Medical Therapy
- Conventional Surgical Therapy
- Minimally Invasive Therapy
The dynamic component of prostatic obstruction explains the variable nature of the symptoms experienced by patients. The prostatic stroma, composed of smooth muscle and collagen, is rich in adrenergic nerve supply. The level of autonomic stimulation thus sets a tone to the prostatic urethra. Use of alpha-blocker therapy decreases this tone, resulting in a decrease in outlet resistance.
The irritative voiding complaints (see below) of BPH result from the secondary response of the bladder to the increased outlet resistance. Bladder outlet obstruction leads to detrusor muscle hypertrophy and hyperplasia as well as collagen deposition. Although the latter is most likely responsible for a decrease in bladder compliance, detrusor instability is also a factor. On gross inspection, thickened detrusor muscle bundles are seen as trabeculation on cystoscopic examination. If left unchecked, mucosal herniation between detrusor muscle bundles ensues, causing diverticula formation (so-called false diverticula composed of only mucosa and serosa).
Benign Prostatic Hyperplasia Clinical Findings
A. Symptoms
As discussed above, the symptoms of BPH can be divided into obstructive and irritative complaints. Obstructive symptoms include hesitancy, decreased force and caliber of stream, sensation of incomplete bladder emptying, double voiding (urinating a second time within 2 h of the previous void), straining to urinate, and post-void dribbling. Irritative symptoms include urgency, frequency, and nocturia.
The self-administered questionnaire developed by the American Urological Association (AUA) is both valid and reliable in identifying the need to treat patients and in monitoring their response to therapy. The AUA Symptom Score questionnaire (Table 22-1) is perhaps the single most important tool used in the evaluation of patients with BPH and is recommended for all patients before the initiation of therapy. This assessment focuses on 7 items that ask patients to quantify the severity of their obstructive or irritative complaints on a scale of 0-5. Thus, the score can range from 0 to 35. A symptom score of 0-7 is considered mild, 8-19 is considered moderate, and 20-35 is considered severe. The relative distribution of scores for BPH patients and control subjects is, respectively, 20% and 83% in those with mild scores, 57% and 15% in those with moderate scores, and 23% and 2% in those with severe scores (McConnell et al, 1994).
A detailed history focusing on the urinary tract excludes other possible causes of symptoms that may not result from the prostate, such as urinary tract infection, neurogenic bladder, urethral stricture, or prostate cancer.
B. Signs
A physical examination, DRE, and focused neurologic examination are performed on all patients. The size and consistency of the prostate is noted, even though prostate size, as determined by DRE, does not correlate with severity of symptoms or degree of obstruction. BPH usually results in a smooth, firm, elastic enlargement of the prostate. Induration, if detected, must alert the physician to the possibility of cancer and the need for further evaluation (ie, prostate-specific antigen [PSA], transrectal ultrasound, and biopsy).
C. Laboratory Findings
A urinalysis to exclude infection or hematuria and serum creatinine measurement to assess renal function are required. Renal insufficiency may be observed in 10% of patients with prostatism and warrants upper-tract imaging. Patients with renal insufficiency are at an increased risk of developing postoperative complications following surgical intervention for BPH. Serum PSA is considered optional, but most physicians will include it in the initial evaluation. PSA, compared with DRE alone, certainly increases the ability to detect CaP, but because there is much overlap between levels seen in BPH and CaP, its use remains controversial (see Screening for CaP).
D. Imaging
Upper-tract imaging (intravenous pyelogram or renal ultrasound) is recommended only in the presence of concomitant urinary tract disease or complications from BPH (eg, hematuria, urinary tract infection, renal insufficiency, history of stone disease).
E. Cystoscopy
Cystoscopy is not recommended to determine the need for treatment but may assist in choosing the surgical approach in patients opting for invasive therapy.
F. Additional Tests
Cystometrograms and urodynamic profiles are reserved for patients with suspected neurologic disease or those who have failed prostate surgery. Measurement of flow rate, determination of post-void residual urine, and pressure-flow studies are considered optional.
Benign Prostatic Hyperplasia Differential Diagnosis
Other obstructive conditions of the lower urinary tract, such as urethral stricture, bladder neck contracture, bladder stone, or CaP, must be entertained when evaluating men with presumptive BPH. A history of previous urethral instrumentation, urethritis, or trauma should be elucidated to exclude urethral stricture or bladder neck contracture. Hematuria and pain are commonly associated with bladder stones. CaP may be detected by abnormalities on the DRE or an elevated PSA (see below).
A urinary tract infection, which can mimic the irritative symptoms of BPH, can be readily identified by urinalysis and culture; however, a urinary tract infection can also be a complication of BPH. Although irritative voiding complaints are also associated with carcinoma of the bladder, especially carcinoma in situ, the urinalysis usually shows evidence of hematuria. Likewise, patients with neurogenic bladder disorders may have many of the signs and symptoms of BPH, but a history of neurologic disease, stroke, diabetes mellitus, or back injury may be present as well. In addition, examination may show diminished perineal or lower extremity sensation or alterations in rectal sphincter tone or the bulbocavernosus reflex. Simultaneous alterations in bowel function (constipation) might also alert one to the possibility of a neurologic origin.
Benign Prostatic Hyperplasia Treatment
After patients have been evaluated, they should be informed of the various therapeutic options for BPH. It is advisable for patients to consult with their physicians to make an educated decision on the basis of the relative efficacy and side effects of the treatment options.
Specific treatment recommendations can be offered for certain groups of patients. For those with mild symptoms (symptom score 0-7), watchful waiting only is advised. On the other end of the therapeutic spectrum, absolute surgical indications include refractory urinary retention (failing at least one attempt at catheter removal), recurrent urinary tract infection from BPH, recurrent gross hematuria from BPH, bladder stones from BPH, renal insufficiency from BPH, or large bladder diverticula (McConnell et al, 1994).
A. Watchful Waiting
Very few studies on the natural history of BPH have been reported. The risk of progression or complications is uncertain. However, in men with symptomatic BPH, it is clear that progression is not inevitable and that some men undergo spontaneous improvement or resolution of their symptoms.
Retrospective studies on the natural history of BPH are inherently subject to bias, related to patient selection and the type and extent of follow-up. Very few prospective studies addressing the natural history of BPH have been reported. Recently, a large randomized study compared finasteride with placebo in men with moderately to severely symptomatic BPH and enlarged prostates on DRE (McConnell et al, 1998). Patients in the placebo arm of the study had a 7% risk of developing urinary retention over 4 years.
As mentioned above, watchful waiting is the appropriate management of men with mild symptom scores (0-7). Men with moderate or severe symptoms can also be managed in this fashion if they so choose. Neither the optimal interval for follow-up nor specific endpoints for intervention have been defined.
B. Medical Therapy
1. Alpha blockers - The human prostate and bladder base contains alpha-1-adrenoreceptors, and the prostate shows a contractile response to corresponding agonists. The contractile properties of the prostate and bladder neck seem to be mediated primarily by the subtype α1a receptors. Alpha blockade has been shown to result in both objective and subjective degrees of improvement in the symptoms and signs of BPH in some patients. Alpha blockers can be classified according to their receptor selectivity as well as their half-life (Table 22-2).
Phenoxybenzamine and prazosin have comparable efficacy with respect to symptomatic relief, but the higher side-effect profile of phenoxybenzamine, associated with its lack of alpha-receptor specificity, precludes its use in BPH patients. Dose titration is necessary with prazosin, with typical therapy started at 1 mg at bedtime for 3 nights, then increased to 1 mg twice a day, which is titrated up to 2 mg twice a day if necessary. At higher doses, little additional symptomatic improvement is observed and side-effect profiles worsen. Typical side effects include orthostatic hypotension, dizziness, tiredness, retrograde ejaculation, rhinitis, and headache.
Long-acting alpha blockers make once-a-day dosing possible, but dose titration is still necessary. Terazosin is initiated at 1 mg daily for 3 days and increased to 2 mg daily for 11 days and then to 5 mg per day. Dosage can be escalated to 10 mg daily if necessary. Therapy with doxazosin is started at 1 mg daily for 7 days and increased to 2 mg daily for 7 days, and then to 4 mg daily. Dosage can be escalated to 8 mg daily if necessary. Side effects are similar to those described for prazosin.
The most recent advance in alpha-blocker therapy is related to the identification of subtypes of alpha-1-receptors. Selective blockade of the α1a receptors, which are localized in the prostate and bladder neck, results in fewer systemic side effects (orthostatic hypotension, dizziness, tiredness, rhinitis, and headache), thus obviating the need for dose titration. Tamsulosin is initiated at 0.4 mg daily and can be increased to 0.8 mg daily if necessary.
Several randomized, double-blind, placebo-controlled trials, individually comparing terazosin, doxazosin, or tamsulosin with placebo, have demonstrated the safety and efficacy of all of these agents. Comparative trials of various alpha blockers are ongoing.
2. 5α-Reductase inhibitors - Finasteride is a 5α-reductase inhibitor that blocks the conversion of testosterone to dihydrotestosterone. This drug affects the epithelial component of the prostate, resulting in a reduction in the size of the gland and improvement in symptoms. Six months of therapy are required to see the maximum effects on prostate size (20% reduction) and symptomatic improvement.
Several randomized, double-blind, placebo-controlled trials have compared finasteride with placebo. Efficacy, safety, and durability are well established. However, symptomatic improvement is seen only in men with enlarged prostates (> 40 cm3). Side effects include decreased libido, decreased ejaculate volume, and impotence. Serum PSA is reduced by approximately 50% in patients being treated with finasteride, but individual values may vary, thus complicating cancer detection.
A recent report suggests that finasteride therapy may decrease the incidence of urinary retention and the need for surgical intervention in men with enlarged prostates and moderate to severe symptoms (McConnell et al, 1998). However, optimal identification of appropriate patients for prophylactic therapy remains to be determined.
3. Combination therapy - The first randomized, double-blind, placebo-controlled study investigating combination alpha-blocker and 5α-reductase inhibitor therapy was recently reported (Lepor et al, 1996). This was a four-arm Veterans Administration Cooperative Trial comparing placebo, finasteride alone, terazosin alone, and combination finasteride and terazosin. Over 1200 patients participated, and significant decreases in symptom score and increases in urinary flow rates were seen only in the arms containing terazosin. However, one must note that enlarged prostates were not an entry criterion; in fact, prostate size in this study was much smaller than that in previous controlled trials using finasteride (32 versus 52 cm3). Additional combination therapy trials are ongoing.
4. Phytotherapy - Phytotherapy refers to the use of plants or plant extracts for medicinal purposes. The use of phytotherapy in BPH has been popular in Europe for years, and its use in the United States is growing as a result of patient-driven enthusiasm. Several plant extracts have been popularized, including the saw palmetto berry, the bark of Pygeum africanum, the roots of Echinacea purpurea and Hypoxis rooperi, pollen extract, and the leaves of the trembling poplar. The mechanisms of action of these phytotherapies are unknown, and the efficacy and safety of these agents have not been tested in multicenter, randomized, double-blind, placebo-controlled studies.
C. Conventional Surgical Therapy
1. Transurethral resection of the prostate (TURP) - Ninety-five percent of simple prostatectomies can be done endoscopically. Most of these procedures involve the use of a spinal anesthetic and require a 1- to 2-day hospital stay. Symptom score and flow rate improvement with TURP is superior to that of any minimally invasive therapy. The length of hospital stay of patients undergoing TURP, however, is greater. Much controversy revolves around possible higher rates of morbidity and mortality associated with TURP in comparison with those of open surgery, but the higher rates observed in one study were probably related to more significant comorbidities in the TURP patients than in the patients undergoing open surgery. Several other studies could not confirm the difference in mortality when results were controlled for age and comorbidities. Risks of TURP include retrograde ejaculation (75%), impotence (5-10%), and incontinence (< 1%). Complications include bleeding, urethral stricture or bladder neck contracture, perforation of the prostate capsule with extravasation, and if severe, TUR syndrome resulting from a hypervolemic, hyponatremic state due to absorption of the hypotonic irrigating solution. Clinical manifestations of the TUR syndrome include nausea, vomiting, confusion, hypertension, bradycardia, and visual disturbances. The risk of the TUR syndrome increases with resection times over 90 min. Treatment includes diuresis and, in severe cases, hypertonic saline administration.
2. Transurethral incision of the prostate - Men with moderate to severe symptoms and a small prostate often have posterior commissure hyperplasia (elevated bladder neck). These patients will often benefit from an incision of the prostate. This procedure is more rapid and less morbid than TURP. Outcomes in well-selected patients are comparable, although a lower rate of retrograde ejaculation with transurethral incision has been reported (25%). The technique involves two incisions using the Collins knife at the 5 and 7 o'clock positions. The incisions are started just distal to the ureteral orifices and are extended outward to the verumontanum.
3. Open simple prostatectomy - When the prostate is too large to be removed endoscopically, an open enucleation is necessary. What constitutes "too large" is subjective and will vary depending upon the surgeon's experience with TURP. Glands over 100 g are usually considered for open enucleation. Open prostatectomy may also be initiated when concomitant bladder diverticulum or a bladder stone is present or if dorsal lithotomy positioning is not possible.
Open prostatectomies can be done with either a suprapubic or retropubic approach. A simple suprapubic prostatectomy is performed transvesically and is the operation of choice in dealing with concomitant bladder pathology. After the bladder is opened, a semicircular incision is made in the bladder mucosa, distal to the trigone. The dissection plane is initiated sharply, and then blunt dissection with the finger is performed to remove the adenoma. The apical dissection should be done sharply to avoid injury to the distal sphincteric mechanism. After the adenoma is removed, hemostasis is attained with suture ligatures, and both a urethral and a suprapubic catheter are inserted before closure.
In a simple retropubic prostatectomy, the bladder is not entered. Rather, a transverse incision is made in the surgical capsule of the prostate, and the adenoma is enucleated as described above. Only a urethral catheter is needed at the end of the procedure.
D. Minimally Invasive Therapy
1. Laser therapy - Many different techniques of laser surgery for the prostate have been described. Two main energy sources of lasers have been utilized - Nd:YAG and holmium:YAG.
Several different coagulation necrosis techniques have been described. Transurethral laser-induced prostatectomy (TULIP) is done with transrectal ultrasound guidance. The TULIP device is placed in the urethra, and transrectal ultrasound is used to direct the device as it is slowly pulled from the bladder neck to the apex. The depth of treatment is monitored with ultrasound.
Most urologists prefer to use visually directed laser techniques. Visual coagulative necrosis techniques have been popularized by Kabalin. Under cystoscopic control, the laser fiber is pulled through the prostate at several designated areas, depending upon the size and configuration of the prostate. Four quadrant and sextant approaches have been described for lateral lobes, with additional treatments directed at enlarged median lobes. Coagulative techniques do not create an immediate visual defect in the prostatic urethra, but rather tissue is sloughed over the course of several weeks and up to 3 months following the procedure.
Visual contact ablative techniques are more time-consuming procedures because the fiber is placed in direct contact with the prostate tissue, which is vaporized. An immediate defect is obtained in the prostatic urethra, similar to that seen during TURP.
Interstitial laser therapy places fibers directly into the prostate, usually under cystoscopic control. At each puncture, the laser is fired, resulting in submucosal coagulative necrosis. This technique may result in fewer irritative voiding symptoms, because the urethral mucosa is spared and prostate tissue is resorbed by the body rather than sloughed.
Advantages of laser surgery include (1) minimal blood loss, (2) rare instances of TUR syndrome, (3) ability to treat patients receiving anticoagulation therapy, and (4) ability to be done as an outpatient procedure. Disadvantages include (1) lack of availability of tissue for pathologic examination, (2) longer postoperative catheterization time, (3) more irritative voiding complaints, and (4) high cost of laser fibers and generators.
Large-scale, multicenter, randomized studies with long-term follow-up are needed to compare laser prostate surgery with TURP and other forms of minimally invasive surgery.
2. Transurethral electrovaporization of the prostate - Transurethral electrovaporization uses the standard resectoscope but replaces a conventional loop with a variation of a grooved rollerball. High current densities cause heat vaporization of tissue, resulting in a cavity in the prostatic urethra. Because the device requires slower sweeping speeds over the prostatic urethra, and the depth of vaporization is approximately one-third of a standard loop, the procedure usually takes longer than a standard TURP. Long-term comparative data are needed.
3. Hyperthermia - Microwave hyperthermia is most commonly delivered with a transurethral catheter. Some devices cool the urethral mucosa to decrease the risk of injury. However, if temperatures do not exceed 45 °C, cooling is unnecessary. Improvement in symptom score and flow rate is obtained, but as with laser surgery, large-scale, randomized studies with long-term follow-up are needed to assess durability and cost-effectiveness.
4. Transurethral needle ablation of the prostate - Transurethral needle ablation uses a specially designed urethral catheter that is passed into the urethra. Interstitial radiofrequency needles are then deployed from the tip of the catheter, piercing the mucosa of the prostatic urethra. The use of radio frequencies to heat the tissue results in a coagulative necrosis. This technique is not adequate treatment for bladder neck and median lobe enlargement. Subjective and objective improvement in voiding occurs, but as mentioned above, comparative long-term randomized studies are lacking.
5. High-intensity focused ultrasound - High-intensity focused ultrasound is another means of performing thermal tissue ablation. A specially designed, dual-function ultrasound probe is placed in the rectum. This probe allows transrectal imaging of the prostate and also delivers short bursts of high-intensity focused ultrasound energy, which heats the prostate tissue and results in coagulative necrosis. Bladder neck and median lobe enlargement are not adequately treated with this technique. Although ongoing clinical trials demonstrate some improvement in symptom score and flow rate, the durability of response is unknown.
6. Intraurethral stents - Intraurethral stents are devices that are endoscopically placed in the prostatic fossa and are designed to keep the prostatic urethra patent. They are usually covered by urothelium within 4-6 months after insertion. These devices are typically used for patients with limited life expectancy who are not deemed to be appropriate candidates for surgery or anesthesia. With the advent of other minimally invasive techniques requiring minimal anesthesia (conscious sedation or prostatic blocks), their application has become more limited.
7. Transurethral balloon dilation of the prostate - Balloon dilation of the prostate is performed with specially designed catheters that enable dilation of the prostatic fossa alone or the prostatic fossa and bladder neck. The technique is most effective in small prostates (< 40 cm3). Although it may result in improvement in symptom score and flow rates, the effects are transient and the technique is rarely used today.