Health Centers > Cancer Health Center > Laryngeal Cancer
Laryngeal cancer
Most common cancer representing <1% of all malignant lesions. Squamous cell carcinomas constitute 5-98% of all malignant neoplasms of the larynx.
- Less than 2% of all carcinomas
- At the time of diagnosis, 62% will have local disease, 26% regional disease, and 8% distant disease in the lungs, liver, and/or bone.
- No racial predilection
- System(s) Affected: Pulmonary
- Synonym(s): Cancer of larynx
Laryngeal cancer
Anatomy
Pathology
General Prevention
Epidemiology
Incidence
Etiology
Associated conditions
Diagnosis
Signs and Symptoms
Tests
Differential Diagnosis
Clinical Findings
T STAGE: Laryngeal Cancer
Treatment
¬ Diet
¬ Activity
¬ Medication
¬ Surgery
Complications
Prognosis
References
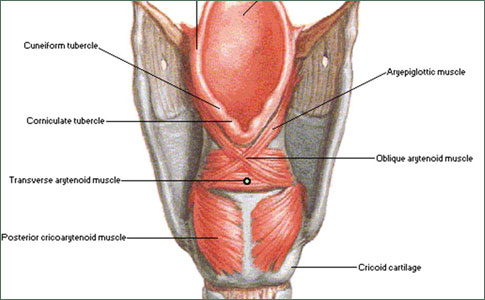
Anatomy
The larynx is composed of three anatomic subsites. The supraglottic larynx extends from the epiglottis superiorly to the false cords inferiorly. Sites within the supraglottic larynx include the epiglottis (both lingual and laryngeal surfaces), aryepiglottic folds, arytenoids, and false cords. The glottic larynx consists of the true vocal cords (including the anterior commissure) superiorly and tissues within 5 mm of the inferior surface of the true vocal cords inferiorly. The subglottic larynx extends from the glottis superiorly to the inferior border of the cricoid cartilage inferiorly. Subglottic cancers are uncommon, accounting for less than 1% of all laryngeal cancers. Subglottic extension of a glottic cancer is more common.
Pathology
Squamous cell carcinoma of the supraglottic larynx accounts for 35% of laryngeal cancers. Fifty percent of these patients will present with cervical lymph node metastases. Lymphatic channels drain to the upper, mid, and lower jugular nodes (levels II, III, and IV). Local spread of cancer is usually in a superior or lateral direction. Inferior spread to the anterior commissure is less common.
Cancer of the glottic larynx accounts for nearly 65% of laryngeal cancers. It tends to be well differentiated, to grow slowly, and to metastasize late. Because the true cords have very limited lymphatic drainage, cervical lymph node metastases occur in only 10% of cases. Cervical lymph node metastases usually occur when the cancer infiltrates beyond the limits of the true cord. Submucosal extension occurs early and can lead to involvement of the anterior commissure and the contralateral vocal cord. The cancer can extend laterally, resulting in cartilage destruction, or superiorly, with involvement of the false vocal cords and aryepiglottic folds (transglottic carcinoma). Subglottic extension can also occur.
Subglottic cancers or subglottic extensions of a glottic cancer are associated with a high incidence of cervical lymph node metastases. Lymphatics from the subglottic larynx drain to the mid and lower jugular lymph nodes (levels III and IV) and to the prelaryngeal (cricothyroid or delphian) node. Subsequently, the pretracheal and paratracheal lymph nodes can be involved.
Anal Cancer: Strategies in Management
The management of anal cancer underwent an interesting transformation over the last two decades.
General Prevention
- Indirect laryngoscopy for patients with persistent hoarseness lasting beyond 1-2 weeks
- Cessation of smoking and/or alcohol abuse
Epidemiology
- Predominant age:
- Median age of occurrence in the sixth and seventh decades
- Less than 1% of laryngeal cancers arise in patients younger than 30 years of age.
- Very rare in young patients, in general
- Predominant sex: Male > female (5:1), however, increasing incidence in women who smoke
Incidence
5 in 100,000 (12,500 new cases per year)
Etiology
- Smoking
- Alcohol abuse
Associated conditions
>10% of patients may have a synchronous squamous cell carcinoma in the lower or upper aerodigestive tract, most notably in the esophagus or lungs.
Diagnosis
Signs and Symptoms
- Persistent hoarseness in an elderly or middle-aged cigarette smoker
- Dyspnea and stridor
- Ipsilateral otalgia
- Dysphagia
- Odynophagia
- Chronic cough
- Hemoptysis
- Weight loss owing to poor nutrition
- Halitosis owing to tumor necrosis
- Mass in the neck from metastatic lymph node
- Laryngeal tenderness owing to tumor necrosis or suppuration
- Lump in the neck
- Broadening of the larynx on palpation with loss of crepitation
- Tenderness of the larynx
- Fullness of the cricothyroid membrane
Tests
Lab
Liver function studies to rule out metastatic disease
Imaging
- Computed tomography (CT) or magnetic resonance imaging if chest and liver or brain metastasis suspected
- Bone scan if bone metastasis suspected
- Screening chest radiograph to rule out metastatic disease
- Laryngoscopy: Fungating, friable tumor with heaped-up edges and granular appearance, with multiple areas of central necrosis and exudate surrounding areas of hyperemia
- Indirect and/or direct laryngoscopy and biopsy to determine stage of disease as well as histologic confirmation
Differential Diagnosis
- Acute or chronic laryngitis
- Benign vocal cord lesions such as polyps, nodules, and papillomas
- Tuberculosis or fungal infection of the larynx
Clinical Findings
The initial presenting symptoms of cancer of the larynx depend upon the site involved. Supraglottic cancers tend to present late with symptoms of dysphagia, odynophagia, hemoptysis, or referred otalgia. Stridor and hoarseness are late findings. Palpable cervical lymphadenopathy is a common presenting sign. Glottic cancers often present early with hoarseness, and palpable lymphadenopathy is uncommon. Late symptoms include dysphagia, odynophagia, stridor, or cough. Subglottic cancer presents with dyspnea, stridor, or palpable cervical lymphadenopathy.
T STAGE: LARYNGEAL CANCER
Supraglottis T1 Tumor limited to one subsite of the supraglottis with normal vocal cord mobility T2 Tumor invades more than one subsite of the supraglottis or glottis, with normal vocal cord mobility T3 Tumor limited to the larynx with vocal cord fixation and/or invades the postcricoid area, medial wall of the piriform sinus, or pre-epiglottic tissues T4 Tumor invades through the thyroid cartilage and/or extends to other tissues beyond the larynx (eg, to the oropharynx or soft tissues of the neck) Glottis T1 Tumor limited to the vocal cord(s) (may involve anterior or posterior commissures) with normal mobility T1a: Tumor limited to one vocal cord T1b:Tumor involves both vocal cords T2 Tumor extends to the supraglottis and/or subglottis, and/or with impaired vocal cord mobility T3 Tumor limited to the larynx with vocal cord fixation T4 Tumor invades through the thyroid cartilage and/or extends to other tissues beyond the larynx (eg, to the oropharynx or soft tissues of the neck) Subglottis T1 Tumor limited to the subglottis T2 Tumor extends to the vocal cord(s) with normal or impaired vocal cord mobility T3 Tumor limited to the larynx with vocal cord fixation T4 Tumor invades through the thyroid cartilage and/or extends to other tissues beyond the larynx (eg, to the oropharynx or soft tissues of the neck)
Treatment
T1 and T2 cancers of the supraglottic and glottic larynx respond well to radiation therapy. Survival rates are similar to those achieved with surgery, including laser excision, but without the attendant morbidity. Elective radiation therapy to the neck is given to patients with supraglottic carcinomas. T3 and T4 cancers of the supraglottic and glottic larynx are treated with a combination of cisplatin-based chemotherapy and radiation therapy in an effort to avoid the morbidity associated with total laryngectomy. Patients are reevaluated following initial chemotherapy and radiation therapy. If there is complete disappearance of the cancer and biopsies are negative, surgery is avoided. In this way, nearly two-thirds of patients can be spared laryngectomy. Survival rates for patients receiving initial chemotherapy and radiation therapy are the same as those for patients receiving total laryngectomy.
Surgical options for supraglottic and glottic cancer include partial laryngectomy or total laryngectomy. Partial laryngectomy is appropriate for patients with T1 and T2 cancers. Vertical partial laryngectomy removes the ipsilateral vocal cord and overlying laryngeal cartilage. The procedure can be extended superiorly to include the ipsilateral false cord or posteriorly to include the ipsilateral arytenoid cartilage. It is an appropriate procedure for patients with reduced cord mobility due to cancer bulk but not for patients with reduced cord mobility due to invasion of the intrinsic musculature. Horizontal partial laryngectomy is indicated for patients with cancers arising above the level of the true cords. All patients will have some degree of aspiration following this procedure, but careful patient selection can minimize the long-term consequences. Total laryngectomy is appropriate therapy for some patients with T3 laryngeal cancers and for most patients with T4 cancers. In this situation, wide field laryngectomy includes removal of the bilateral level II, III, and IV cervical lymph nodes. Ipsilateral thyroid lobectomy is performed to facilitate paratracheal lymph node dissection.
The presence of cervical lymph node metastases is an indication for radical or modified neck dissection. Elective neck dissection or radiation therapy is not indicated for T1 and T2 glottic cancers but is indicated for all supraglottic cancers and for T3 and T4 glottic cancers. If the primary cancer is treated by surgery, an elective neck dissection is appropriate unless adjuvant radiation therapy to the primary cancer site is planned. In that case, elective neck radiation therapy can be given and the neck dissection deferred. If the primary cancer is treated with radiation therapy, elective neck radiation therapy is appropriate and operative dissection can be deferred.
Diet
- Nasogastric or gastrostomy feeding may be necessary if tumor involves esophageal inlet.
- No special diet otherwise
Activity
Patient may remain fully active unless he or she is debilitated from more advanced disease and/or greater degree of surgery.
Medication (Drugs)
- Narcotics may be necessary for pain control during treatment for mucositis secondary to radiation therapy.
- Nystatin mouth rinses for oral thrush
Surgery
- Tracheotomy may be necessary if tumor is large enough to cause upper airway obstruction
- Early disease may be treatable by either radiation therapy or laser cordectomy on an outpatient basis. Ninety percent cure rates are the rule.
- More advanced disease needs inpatient care necessitating partial or total laryngectomy and postoperative radiation therapy 4-5 weeks after surgery, depending on the stage of disease.
The Larynx - laryngeal cancers treatment
Because of the prominent role the larynx plays in communication, swallowing, respiration, protection of the lower airway, and therefore, quality of life, the treatment of cancer of the larynx presents formidable dilemmas regarding the functional consequences of treatment in addition to the intrinsic threat to life posed by these cancers. Unique to this particular site of head and neck cancer, quality-of-life issues have been incorporated into treatment decision making more extensively than for other cancer sites. Cancer of the larynx is generally diagnosed at an earlier stage than are other head and neck sites, primarily owing to the early manifestation of symptoms. As a result, cure rates are generally higher than for other sites.
Read more » »
Complications
- Temporary odynophagia or dysphagia secondary to mucositis and/or thrush during radiation therapy
- Persistent hoarseness despite adequate treatment, necessitating further adjunctive procedures and/or speech therapy
- Tracheostomal stenosis requiring stenting with laryngectomy tubes or further surgery
- Dysphagia secondary to upper esophageal stricture after total laryngectomy, necessitating dilatation
- Aspiration after partial laryngectomy, necessitating complete laryngectomy or tracheotomy
- Inability to decannulate after partial laryngectomy because of laryngeal stenosis and/or aspiration
- Radiation-induced chondronecrosis, which mimics tumor recurrence
- Radiation edema, necessitating emergent tracheotomy
Prognosis
Five-year survival rates for supraglottic cancer with appropriate treatment are as follows: stage I, 90-95%; stage II, 75-80%; stage III, 50%; stage IV, 20-40%.
Five-year survival rates for glottic cancer with appropriate treatment are as follows: stage I, 80-95%; stage II, 70-80%; stage III, 50-70%; stage IV, 20-50%.
References
- Forastiere AA et al: Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med 2003;349:2091. Pubmed: 14645636
- Hinerman RW et al: Carcinoma of the supraglottic larynx: treatment results with radiotherapy alone or with planned neck dissection. Head Neck 2002;24:456. Pubmed: 12001076
- Hinerman RW et al: Early laryngeal cancer. Curr Treat Options Oncol 2002;3:3. Pubmed: 12057082
- Mendenhall WM et al: Management of T1-T2 glottic carcinomas. Cancer 2004;100:1786. Pubmed: 15112257
- Ariyan S. Cancer of the Head and Neck. St. Louis, MO: Mosby; 1987.
- Cummings CW, et al., eds. Otolaryngology Head and Neck Surgery. Vol 3. 3rd ed. New York, NY: Mosby; 1998.
- Suen JY, Myers EN. Cancer of the Head and Neck. 3rd ed. Philadelphia, PA: WB Saunders; 1996.