Needle biopsy underused in breast cancer diagnosis, negatively impacting diagnosis and care
Needle biopsy, the standard of care radiological procedure for diagnosing breast cancer, is underused with too many patients undergoing the more invasive, excisional biopsy to detect their disease, according to research from The University of Texas MD Anderson Cancer Center.
The study, published in the Journal of Clinical Oncology, also finds that patients are often influenced by surgeons to undergo the unnecessary surgery - a decision that’s costly and can negatively impact their diagnosis and treatment.
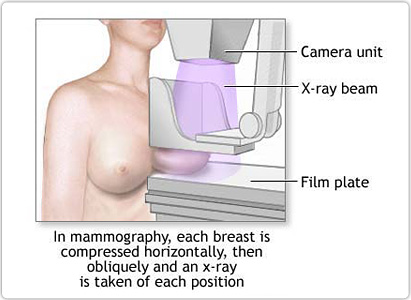
A needle biopsy is a non-surgical procedure typically performed by a radiologist that uses a thin needle to remove sample tissue from the breast. The procedure was originally endorsed as a reasonable standard of care in 1997 by a Joint Task Force comprising the American College of Surgeons (ACS), College of American Pathologists and American College of Radiologists.
The procedure was endorsed as a quality measure by the ACS in 2006, says Benjamin Smith, MD, associate professor in MD Anderson’s departments of Radiation Oncology and Health Services Research.
“Still too often in my practice, I see patients that come to MD Anderson for care after having an excisional biopsy performed for diagnosis, when they obviously could have had a needle biopsy,” says Smith, the study’s corresponding author. “Often, the excisional biopsy negatively affects other aspects of breast cancer treatment and is simply a wasteful procedure. With this study, we wanted to quantitate the magnitude of that waste on a national scale, and identify some of the impacts of that practice pattern on the well-being of patients.”
For the retrospective study, Smith and his colleagues reviewed Medicare claims of 89,712 patients diagnosed with breast cancer from 2003-2007. All were treated with breast conserving surgery and radiation. The study also identified 11,279 diagnosing surgeons and 12,405 treating surgeons. Of the patients, 68.4 percent (61,353) underwent a needle biopsy, with the rate of those undergoing the procedure increasing from 60.8 percent in 2003 to 76.5 percent in 2007.
 Of the total cohort, 68.4 percent of the patients consulted with a surgeon prior to a biopsy and 31.6 percent saw a surgeon after their biopsy. Of the patients who saw a surgeon upfront: 46.3 percent did not have a needle biopsy; 38.4 percent underwent the procedure, but performed by their surgeon; and 15.4 percent had the needle biopsy performed by a radiologist. In contrast, all patients who saw a surgeon post-biopsy underwent the needle biopsy.
Of the total cohort, 68.4 percent of the patients consulted with a surgeon prior to a biopsy and 31.6 percent saw a surgeon after their biopsy. Of the patients who saw a surgeon upfront: 46.3 percent did not have a needle biopsy; 38.4 percent underwent the procedure, but performed by their surgeon; and 15.4 percent had the needle biopsy performed by a radiologist. In contrast, all patients who saw a surgeon post-biopsy underwent the needle biopsy.
The researchers found that surgeon characteristics associated with excisional biopsy included: lack of board certification; training outside the U.S.; medical school graduation before 1980 and low case volume. Also, patient characteristics most associated with surgeon consultation before biopsy, and thus a lower rate of needle biopsy, were: older age; black race; Medicaid coverage; co-morbid illness; earlier year of diagnosis and rural residence.
Geographical discrepancies in the rate of needle biopsies performed were noted - the researchers contrast the low rate of 24.1 percent in Bismarck, North Dakota to a high of 97.2 percent in Lynchburg, Virginia. Yet, Smith notes that access issues were far less of a factor for the decision than that of the surgeon’s influence.
“The real question is the role of the surgeon and to understand that influence. With our study, we set up a statistical model that allowed us to compare the impact of patient-to-surgeon factors. While there are access issues that should be addressed, it’s clear that the surgeon’s role is very important for the patients’ care,” explains Smith.
Excisional biopsies were negatively associated with multiple breast cancer surgeries, 69.6 percent, compared to 33.7 percent of those who did not undergo the surgery.
For patients, says Smith, it’s important to know that needle biopsy is considered the standard of care for breast cancer diagnosis, it’s relatively readily accessible, and there are possible medical benefits of making the right decision - such as preventing additional surgeries and enduring fewer complications.
“An open surgical biopsy actually makes lymph node biopsy less accurate - and lymph node status is the most important factor when making critical decisions about adjuvant therapy. So breast cancer patients should be fully educated that this is the standard of care and ask for it,” stressed Smith.
“For physicians, I think our findings suggest an opportunity to educate and encourage them to do the right thing in the best interest of their patient,” Smith continued.
In addition to Smith, authors from MD Anderson include: Thomas A. Buchholz, M.D., Executive Vice President and Physician-In-Chief; Sharon H. Giordano, M.D., Ying Xu, M.D., Linda Elting, DRPH, Chan Shen, Ph.D., and Jing Jiang, all with Health Services Research; Grace L. Smith, M.D., Radiation Oncology ; Gary J. Whitman, M.D., Diagnostic Radiology; Yu Shen, Ph.D., Biostatistics; Wei Yang, M.D., Diagnostic Radiology; Kelly K. Hunt, M.D., and Dalliah M. Black, M.D., both with Surgical Oncology. Jan M. Eberth, Arnold School of Public Health, University of South Carolina, is the study’s first author.
The study was supported by grants from the following: Cancer Prevention and Research Institute of Texas; the Cancer Prevention Training Program at MD Anderson; the American Cancer Society; Multidisciplinary Postdoctoral Awards from the Department of Defense; and from the National Cancer Institute, grant numbers CA16672 and T32CA77050.
###
Laura Sussman
713-745-2457
832-264-8893
.(JavaScript must be enabled to view this email address)
MD Anderson Communications Office
713-792-0655
.(JavaScript must be enabled to view this email address)