New way to predict response to chemo in triple-negative breast cancer
Researchers from University Hospitals (UH) Case Medical Center’s Seidman Cancer Center will present findings from a study that found the presence of tumor-infiltrating lymphocytes, a type of white blood cell, ahead of treatment may help predict response to platinum-based chemotherapy in women with triple-negative breast cancer. The data are being presented at the 50th American Society for Clinical Oncology (ASCO) Annual Meeting in Chicago.
“Triple-negative breast cancers tend to be more aggressive compared to other types of breast cancers, and being able to predict response to therapy could greatly impact treatment decisions and patient outcomes,” says study author Shaveta Vinayak, MD, oncologist at UH Case Medical Center and Assistant Professor at Case Western Reserve University School of Medicine. “Our research shows that the presence of lymphocytes before administering chemotherapy could predict a positive response to platinum-based therapy.”
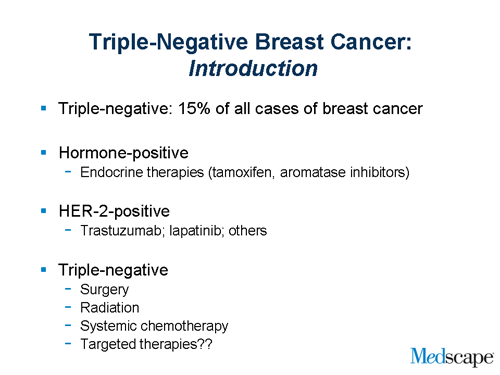
Triple negative breast cancers are those that do not have estrogen or progesterone receptors, and do not have an excess of the HER2 protein on the cancer cell surfaces. This makes it more difficult to treat because the hormone-blocking or the HER2-targeting treatments do not work. Triple negative breast cancers tend to occur more often in younger women and in African-American women.
Platinum-based therapies are being tested in clinical trials for triple-negative breast cancer, and evaluation of tumor-infiltrating lymphocytes is an important factor in determining response to this treatment. For oncologists, this could provide a new tool to individualize treatment for these women.
Researchers from various institutions in the Eastern Cooperative Oncology Group, one of the largest clinical cancer research organizations in the United States that conducts clinical trials in all types of adult cancers, contributed to this analysis. Funding for this study was provided by Breast Cancer Research Foundation, ASCO Conquer Cancer Foundation, Triple-Negative Breast Cancer Foundation, Myriad Genetics, and National Institutes of Health (Stanford CTSA).
True or False? There are no good treatments for TNBC.
FALSE! There ARE good treatments for TNBC-it’s just that two of the most common treatments for most types of breast cancer don’t work for TNBC patients.
To be more specific, TNBC cannot be treated with the medications known as tamoxifen, aromatase inhibitors, or trastuzumab. The reason for this is because TNBC does not have the targets known as estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 (Her2) needed for these drugs to work. It is the lack of these targets that lead to the name “triple-negative.”
However, all of the other available therapies for breast cancer-surgery, radiation, and chemotherapy-can do a good job of treating TNBC. In fact, a lot of research has found that the early response to chemotherapy is often better in patients with TNBC than in patients with other types of breast cancer.
The largest of these studies looked at more than 1,000 patients who received presurgical chemotherapy for breast cancer. After treatment, 22% of the patients with TNBC did not have signs of cancer at the original tumor site and surrounding lymph nodes (researchers call this a complete response), while only 11% of patients with other types of breast cancer had the same positive results.
Among patients who had a complete response, survival rates were similar between those with TNBC and those with other types of breast cancer.
Still, this study aside, it is important to know that TNBC is an area of lots of research, and there is a lot of work being done to discover more treatment options.
True or False? TNBC is more likely to relapse than other breast cancers and more likely to be fatal.
Yes, this is true-but only up to a point. Many cases of TNBC are actually low risk. This risk is estimated based on tumor size, involvement of the lymph nodes in the armpit, and other factors that help your doctor determine the chance of recurrence.
In the study mentioned earlier, recurrence (when cancer comes back) and death rates were higher for TNBC patients-but only in the first 3 years after diagnosis and first treatment. The researchers even suggested that the risk of recurrence and death may have been higher for non-TNBC patients in years 4 to 6. This means that, 3 years after diagnosis, those patients who were successfully treated for TNBC had similar-or better-outcomes than patients with other types of breast cancer.
About the Study
Oral Abstract Session
Breast Cancer - Triple-Negative/Cytotoxics/Local Therapy
Abstract #1024: June 3, 9:45 AM - 12:45 PM
Dr. Vinayak will present new findings from the PrECOG 0105 trial, a trial evaluating neoadjuvant platinum-based chemotherapies - carboplatin, gemcitabine and iniparib - in women with triple-negative breast cancer. This correlative study assessed the association of tumor-infiltrating lymphocytes in pre-treatment breast cancer tissue with pathologic response to treatment.
 The trial evaluated 70 patients with triple-negative breast cancer who had completed at least 4 of 6 planned cycles of therapy. Tissue and tumor sections from pre-chemotherapy biopsies were evaluated by a central pathologist for density of lymphocytes. Pathologic response was assessed by the residual cancer burden index.
The trial evaluated 70 patients with triple-negative breast cancer who had completed at least 4 of 6 planned cycles of therapy. Tissue and tumor sections from pre-chemotherapy biopsies were evaluated by a central pathologist for density of lymphocytes. Pathologic response was assessed by the residual cancer burden index.
Results showed that tumor-infiltrating lymphocytes found in the connective tissue and the tumor itself are predictive of response to platinum-based neoadjuvant chemotherapy and are significantly associated with triple-negative breast cancer subtypes, with the highest frequency in the immunomodulatory subtype.
###
About University Hospitals
University Hospitals, the second largest employer in Northeast Ohio, serves the needs of patients through an integrated network of hospitals, outpatient centers and primary care physicians in 16 counties. At the core of our health system is University Hospitals Case Medical Center, one of only 18 hospitals in the country to have been named to U.S. News & World Report’s most exclusive rankings list: the Best Hospitals 2013-14 Honor Roll. The primary affiliate of Case Western Reserve University School of Medicine, UH Case Medical Center is home to some of the most prestigious clinical and research centers of excellence in the nation and the world, including cancer, pediatrics, women’s health, orthopaedics and spine, radiology and radiation oncology, neurosurgery and neuroscience, cardiology and cardiovascular surgery, organ transplantation and human genetics.
 Its main campus includes the internationally celebrated UH Rainbow Babies & Children’s Hospital, ranked among the top children’s hospitals in the nation; UH MacDonald Women’s Hospital, Ohio’s only hospital for women; and UH Seidman Cancer Center, part of the NCI-designated Case Comprehensive Cancer Center at Case Western Reserve University. UH Case Medical Center is the 2012 recipient of the American Hospital Association - McKesson Quest for Quality Prize for its leadership and innovation in quality improvement and safety.
Its main campus includes the internationally celebrated UH Rainbow Babies & Children’s Hospital, ranked among the top children’s hospitals in the nation; UH MacDonald Women’s Hospital, Ohio’s only hospital for women; and UH Seidman Cancer Center, part of the NCI-designated Case Comprehensive Cancer Center at Case Western Reserve University. UH Case Medical Center is the 2012 recipient of the American Hospital Association - McKesson Quest for Quality Prize for its leadership and innovation in quality improvement and safety.
Triple negative breast cancer
Women who develop breast cancer under the age of 40 are more likely to have triple negative breast cancer than older women with breast cancer. Black women with breast cancer are more likely to have triple negative breast cancer than white women with breast cancer.
Many breast cancers have receptors for the hormones oestrogen and progesterone, or less commonly for a protein called HER2. These receptors can stimulate the cancers to grow. After surgery, the tissue that is removed from a woman’s breast is tested for receptors.
Women who have breast cancer with hormone receptors are prescribed hormonal treatments, such as tamoxifen or anastrozole. Women with breast cancers that have high levels of HER2 receptors are given a drug called trastuzumab (Herceptin®).
If you have a breast cancer that doesn’t have any oestrogen, progesterone or HER2 receptors, this is called triple negative breast cancer. Women with triple negative breast cancer don’t benefit from treatment with hormonal therapy or Herceptin. Chemotherapy is more effective for women with triple negative breast cancer.
Causes and risk factors
The risk factors for triple negative breast cancer aren’t clear. Breast cancers that depend on hormones to grow are linked with risk factors to do with having children, such as how old a woman was when she had her first child. Triple negative breast cancer doesn’t seem to share these risk factors.
Most women with triple negative breast cancer don’t have a strong history of breast cancer in their family (hereditary breast cancer). However, some women with triple negative breast cancer have a faulty gene called BRCA1. This gene is inherited from a parent and can cause breast cancer to run in families. Most breast cancers caused by BRCA1 are triple negative.
Diagnosis of triple negative breast cancer
Tests for triple negative breast cancer are the same as tests for any other type of breast cancer. The most important test is removing a small piece of tissue (biopsy) from the breast. The tissue is examined under a microscope for cancer cells. You may also have other tests to find out if the cancer has spread outside the breast.
Staging and grading of triple negative breast can
###
Alicia Reale
.(JavaScript must be enabled to view this email address)
University Hospitals Case Medical Center