MU Study Finds More Accurate Method to Diagnose Pancreatic Cancer
Researchers from the University of Missouri have found a more accurate laboratory method for diagnosing pancreatic cancer, the fourth leading cause of cancer death in the United States. The disease causes more than 38,000 deaths each year in the United States, and kills 94 percent of people with the illness within five years, according to the National Cancer Institute.
“Pancreatic cancer can be difficult to diagnose because of subtle differences that distinguish between healthy tissue, cancerous tissue and tissue that is atypical, or suspicious,” said Lester Layfield, MD, professor and chair of the MU School of Medicine’s Department of Pathology and Anatomical Sciences. “Our goal was to find a way to make a more accurate and reproducible diagnosis.”
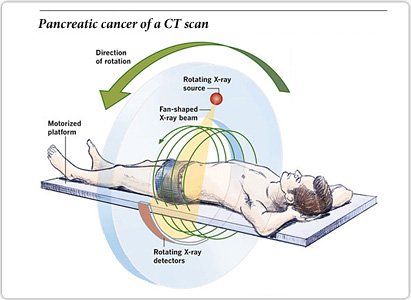
Because of the pancreas’ location within the body, no routine screening methods, such as mammography for breast cancer, exist for detecting pancreatic cancer.
If a physician suspects a patient may have pancreatic cancer, a biopsy of the pancreatic tissue is taken through a minimally invasive technique called endoscopic ultrasound-guided fine-needle aspiration.
“Traditionally, pathologists have examined a tissue sample through a microscope and made a diagnosis based on the overall features of all the cells in the tissue sample,” Layfield said. “Previous research has shown an experienced pathologist can diagnose pancreatic cancer with accuracy in the mid-to-upper 80 percent range using current techniques. However, we wanted to develop a more accurate method by determining which cellular features are most closely associated with cancer.”
 To develop the new diagnostic method, MU researchers performed a retrospective study of the records from 57 patients at University of Missouri Health Care who were tested for pancreatic cancer. They evaluated 16 features of pancreatic biopsies that could be evaluated under a microscope and performed a statistical analysis to determine which could be most reliably identified by multiple pathologists and which were most likely to be associated with pancreatic cancer.
To develop the new diagnostic method, MU researchers performed a retrospective study of the records from 57 patients at University of Missouri Health Care who were tested for pancreatic cancer. They evaluated 16 features of pancreatic biopsies that could be evaluated under a microscope and performed a statistical analysis to determine which could be most reliably identified by multiple pathologists and which were most likely to be associated with pancreatic cancer.
“Through our analysis, we developed a group of four characteristics that allow a pathologist to diagnose pancreatic cancer with 93 percent accuracy — a substantial improvement over the traditional method,” Layfield said. “I believe this new technique can help pathologists improve the diagnosis of pancreatic cancer, ultimately improving care for patients by providing an evidence-based approach to diagnosing the disease and determining the best treatment.”
Pancreatic cancer statistics
Pancreatic cancer statistics are presented here.
In 2010, 8,463 people in the UK were diagnosed with pancreatic cancer.
In 2010 there were 7,901 deaths from pancreatic cancer in the UK.
In 2005-2009, 3.7% of adult pancreatic cancer patients (3.6% of men and 3.8% of women) in England survived their cancer for five years or more.
 The four features of pancreatic cancer the researchers identified are:
The four features of pancreatic cancer the researchers identified are:
a wide variation in the size of pancreatic cells’ nuclei, called anisonucleosis
oversized nucleoli, called macronucleoli
single atypical epithelia cells, a type of cell found in the pancreas
mucinous metaplasia, which is the production of mucin in cells that normally don’t produce the substance
Pancreatic cancer occurs when the cells within the tissues of the pancreas become cancerous. The disease forms in one of two different types of cells: exocrine (cells that make enzymes to aid digestion) and endocrine (hormone-making cells). Exocrine tumors comprise 95 percent of pancreatic cancer cases. The prognosis and treatment of endocrine cancers of the pancreas vary from the more common exocrine cancers because they may have different causes, symptoms, and treatment methods.
Pancreatic cancer is one of the leading causes of cancer-related deaths in Texas, with the death rate increasing over the last decade. The survival rates for pancreatic cancer are lower than most other forms of cancer, with only 6 percent of newly diagnosed patients expected to survive more than five years. The low survival rates can be attributed in part to the lack of symptoms during the early stages of the disease and the lack of a reliable screening test.
Statistics
Pancreatic cancer ranks as the fourth deadliest cancer in the United States after cancers of the lung, colon, and breast.
In 2013, an estimated 45,220 pancreatic cancer new diagnoses and 38,460 deaths are expected in the U.S.
In Texas, an estimated 2,775 new cases of pancreatic cancer will be diagnosed in 2013, with 2,510 deaths expected.
The study, “Risk Stratification Using Morphological Features in Endoscopic-ultrasonography Guided Fine Needle Aspirations of Pancreatic Ductal Adenocarcinoma,” was presented at the American Society for Clinical Pathology’s 2013 annual meeting.
Pancreatic Cancer Risk Factors
Age: The risk of developing pancreatic cancer increases with age, with nearly all patients diagnosed after age 45. The median age of diagnosis is 71.
Race: African Americans face a higher risk of pancreatic cancer than do whites.
Smoking: People who smoke are approximately twice as likely to have pancreatic cancer as nonsmokers.
Obesity: Those who are considered obese face an increased risk of the disease.
Family History: Those with a family history of the disease have an increased risk for pancreatic cancer. In some cases, the incidence of pancreatic cancer in a family may be associated with a genetic mutation. Genetic tests may identify a person’s risk for the disease.
Health Conditions: Pancreatic cancer is more common in diabetics and in some cases the cancer appears to cause the diabetes. Chronic pancreatitis due to a gene mutation; cirrhosis of the liver; and excess stomach acid or the bacteria H. pylori also increase risk.
Industrial Exposure: Increased risk is associated with long-term exposure to some pesticides, dyes, and chemicals.
###
University of Missouri School of Medicine