Stanford scientists identify source of most cases of invasive bladder cancer
A single type of cell in the lining of the bladder is responsible for most cases of invasive bladder cancer, according to researchers at the Stanford University School of Medicine.
Their study, conducted in mice, is the first to pinpoint the normal cell type that can give rise to invasive bladder cancers. It’s also the first to show that most bladder cancers and their associated precancerous lesions arise from just one cell, and explains why many human bladder cancers recur after therapy.
“We’ve learned that, at an intermediate stage during cancer progression, a single cancer stem cell and its progeny can quickly and completely replace the entire bladder lining,” said Philip Beachy, PhD, professor of biochemistry and of developmental biology. “All of these cells have already taken several steps along the path to becoming an aggressive tumor. Thus, even when invasive carcinomas are successfully removed through surgery, this corrupted lining remains in place and has a high probability of progression.”
Although the cancer stem cells, and the precancerous lesions they form in the bladder lining, universally express an important signaling protein called sonic hedgehog, the cells of subsequent invasive cancers invariably do not - a critical switch that appears vital for invasion and metastasis. This switch may explain certain confusing aspects of previous studies on the cellular origins of bladder cancer in humans. It also pinpoints a possible weak link in cancer progression that could be targeted by therapies.
“This could be a game changer in terms of therapeutic and diagnostic approaches,” said Michael Hsieh, MD, PhD, assistant professor of urology and a co-author of the study. “Until now, it’s not been clear whether bladder cancers arise as the result of cancerous mutations in many cells in the bladder lining as the result of ongoing exposure to toxins excreted in the urine, or if it’s due instead to a defect in one cell or cell type. If we can better understand how bladder cancers begin and progress, we may be able to target the cancer stem cell, or to find molecular markers to enable earlier diagnosis and disease monitoring.”
Beachy is the senior author of the study, which will be published online April 20 in Nature Cell Biology. He is the Ernest and Amelia Gallo Professor in the School of Medicine and a member of the Stanford Cancer Institute and the Stanford Institute for Stem Cell Biology and Regenerative Medicine. He is also a Howard Hughes Medical Institute investigator. Kunyoo Shin, PhD, an instructor at the institute, is the lead author.
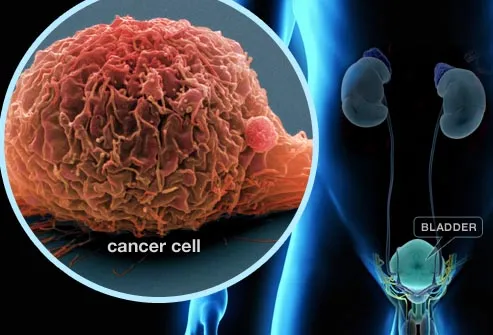 Bladder cancer is the fourth most common cancer in men and the ninth most common in women. Smoking is a significant risk factor. There are two main types of the disease: one that invades the muscle around the bladder and metastasizes to other organs, and another that remains confined to the bladder lining. Unlike the more-treatable, noninvasive cancer - which comprises about 70 percent of bladder cancers - the invasive form is largely incurable. It is expensive and difficult to treat, and the high likelihood of recurrence requires ongoing monitoring after treatment.
Bladder cancer is the fourth most common cancer in men and the ninth most common in women. Smoking is a significant risk factor. There are two main types of the disease: one that invades the muscle around the bladder and metastasizes to other organs, and another that remains confined to the bladder lining. Unlike the more-treatable, noninvasive cancer - which comprises about 70 percent of bladder cancers - the invasive form is largely incurable. It is expensive and difficult to treat, and the high likelihood of recurrence requires ongoing monitoring after treatment.
In 2011, Shin and Beachy and their colleagues identified a cell type in the bladder that is capable of completely replacing the lining of the organ after infection or damage. The fact that it could give rise to multiple cell types (even forming small, multilayered, bladder-like spheres when cultured in vitro), and also self-renew, showed that it was a bladder stem cell. They found that the cell, which came from the basal layer of the bladder epithelium, used a protein called sonic hedgehog to “talk” to other cells in the bladder and stimulate proliferation and specialization into other cell types. (Beachy identified the first hedgehog protein in fruit flies in 1992; the hedgehog signaling pathway has since been shown to play a vital role in embryonic development and in many types of cancers.)
Many animal models of cancer rely on prior knowledge or hunches as to what genes or cell types are involved. Researchers may genetically alter an animal, or a certain cell type, to induce the overexpression of a gene known to be involved in tumorigenesis, for example, or block the expression of a gene that inhibits cancer development.
Although prior work suggested that basal cells may play a role in bladder cancer, the researchers chose an unbiased approach when developing their mouse model that more closely mimicked what happens in humans: They put a chemical compound called N-butyl-N-4-hydroxybutyl nitrosamine, or BBN, in the mice’s drinking water and watched the animals over a period of months.
Nitrosamines are carcinogens found in cigarette smoke; BBN is a form of the chemical that is specifically activated in the bladder. After four months, many of the animals had developed precancerous lesions, or carcinomas in situ, in their bladders that very closely resemble those seen in human patients. By six months, all of the animals had developed invasive bladder cancers.
With their model in place, the researchers then conducted two main experiments in the mice: In the first experiment, they looked to see what would happen in animals exposed to BBN when the sonic-hedgehog-expressing cells were marked with a distinctive fluorescent color. In the second, they used genetic techniques to selectively kill those same cells in animals prior to exposure with BBN.
In the first case, they saw something startling: After just a few months of BBN exposure, nearly the entire lining of the bladder was labeled with the fluorescent green marker that indicated the cells had arisen from the sonic-hedgehog-expressing basal stem cells. When transplanted into other mice, those labeled cells were able to give rise to bladder cancers, but cells not expressing sonic hedgehog did not.
In the second case, no tumors grew in the animals in which the stem cells had been selectively killed - although the bladder architecture became severely compromised in the absence of stem cells to regenerate cells lost during the normal course of bladder function.
“So now we have two lines of evidence indicating that the bladder stem cells are solely responsible for tumorigenesis,” Shin said. “When we mark the bladder stem cells, the tumors are also marked. When we remove, or ablate, the stem cells, no tumors arise after BBN treatment.”
Next the researchers tackled the question of whether bladder cancers arise as the result of genetic changes to one or more of these bladder stem cells. To do so, they used a genetically engineered mouse with cells that fluoresce green, but which can be triggered to randomly fluoresce one of three other colors: red, blue or yellow. Known as a “rainbow mouse,” the animal allows researchers to more precisely determine the origin of groups of cells. If all cells in a tumor are red, for example, it is much more likely that they originated from a single cell.
“After four months of BBN treatment,” Beachy said, “we’d most often see just one color dominating the entire epithelium. This clearly indicates that a single cell has taken over the lining of the entire bladder, elbowing out its neighbors in a way that’s not been seen in other organs.”
Further studies showed that, surprisingly, none of the cells in the most advanced, invasive carcinomas in the BNN-treated animals expressed sonic hedgehog - despite the fact that only sonic-hedgehog-expressing cells are able to give rise to the earlier stages of bladder cancer. One obvious implication of the lack of sonic hedgehog expression in these cells is that the hedgehog pathway somehow inhibits steps required for tissue invasion or metastasis.
“We know that the hedgehog pathway is widely used throughout the animal kingdom to tightly regulate cellular and tissue differentiation,” Hsieh said. “So its loss could make sense in this context because cancer is essentially a loss of normal regulation.”
“One really important lesson from this study,” Beachy said, “is the idea that, by the time you get to a full-blown tumor, the properties of the cells in that tumor may have changed quite significantly from the cell type that gives rise to the tumors. This can complicate understanding how human tumors arise, because even if you identify the tumor-propagating cells within a mature tumor, conclusions about the origins of a cancer based on properties of these cells may be inaccurate.”
###
Other Stanford co-authors of the study were graduate students Agnes Lim and Jared Honeycutt; postdoctoral scholar Justin Odegaard, MD, PhD; and research assistant Sally Kawano.
The study was funded by the National Institutes of Health (grant R01CA157877), a Pathway to Independence Award and the Howard Hughes Medical Institute.
###
Krista Conger
.(JavaScript must be enabled to view this email address)
650-725-5371
Stanford University Medical Center