Muscle-invasive and non-muscle invasive bladder cancers arise from different stem cells
Bladder cancer will kill upward of 170,000 people worldwide this year, but bladder cancer isn’t fatal in the bladder. Instead, in order to be fatal the disease must metastasize to faraway sites. The question has been this: does localized, non-muscle invasive (NMI) bladder cancer eventually become the more dangerous, muscle-invasive (MI) form of the disease, or are NMI and MI bladder cancers genetically distinct from the start?
A University of Colorado Cancer Center study published today in the journal Stem Cells shows it’s the latter: the progenitor cells that create MI bladder cancer are different than the progenitor cells that create NMI bladder cancer. Though these two cancers grow at the same site, they are different diseases.
“This work provides an important new perspective on how we look at bladder cancer biology,” says Dan Theodorescu, MD, PhD, director of the University of Colorado Cancer Center and the study’s senior author.
The group including first author Garrett Dancik, PhD, genetically profiled two cell types that could give rise to bladder cancer - the basal and umbrella layers of the normal bladder lining (urothelium) - to discover the gene signatures specific to each of these cell populations.
Then the group compared these gene signatures to human bladder cancer samples. The tumor samples were distinct: those with the signature of umbrella cells were likely to be lower stage and patients eventually had favorable outcomes; tumors with the signatures of basal layer cells were likely to be higher stage and patients eventually had worse outcomes.
The Facts on Cancer of the Bladder
In cancer of the bladder, certain harmful cells invade the bladder and destroy healthy cells, which cause the bladder not to function properly.
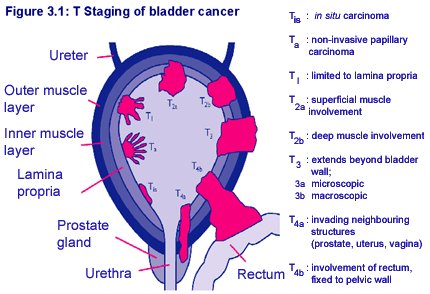
The bladder is a hollow organ that stores urine as it is filtered from the kidneys. The flexible bladder wall is made up of three layers, allowing the bladder to expand and contract as needed. 90% of bladder cancers are found in the epithelial lining, the innermost layer of the wall.
Bladder cancer is the sixth leading cause of new cancer cases in Canada each year. It is diagnosed 2 to 3 times more often in men than in women, and it is seen in Caucasians twice as often as those of African descent. It’s the fourth most common cancer among American men, the ninth most common in women.
Because of early diagnosis and better treatments, the mortality rates for this disease have been falling significantly over the last 25 years.
![]() “We saw a fairly stark difference between these tumor types: those with basal signatures were distinctly more aggressive than those with umbrella signatures,” Theodorescu says. In fact, these signatures predicted tumor stage and patient survival better than many existing prognostic markers.
“We saw a fairly stark difference between these tumor types: those with basal signatures were distinctly more aggressive than those with umbrella signatures,” Theodorescu says. In fact, these signatures predicted tumor stage and patient survival better than many existing prognostic markers.
“Our results suggests that NMI cells arise from non-basal cells, whereas MI tumors arise from basal cells,” Theodorescu says.
Causes of Cancer of the Bladder
The actual cause of bladder cancer is unknown, but there are some proven risk factors. They include:
smoking - smokers are twice as likely to develop bladder cancer than non-smokers
chemical exposure - certain chemicals, such as those used in the following professions, can become concentrated in the urine, creating a risk factor for cancer:
- hairdressers
- painters
- textile workers
- dye, leather, and rubber workers
race - Caucasians have twice as high a risk of developing this cancer as people of African descent; Asians have the lowest risk
gender - men have a 2 to 3 times higher risk than women of developing bladder cancer
age - most cases of bladder cancer are diagnosed in people over the age of 40 years
previous use of certain chemotherapy medications, such as cyclophosphamide* (often used in breast cancer and lymphoma treatment), can significantly increase the risk of later developing bladder cancer
previous radiation to the pelvic area
family or personal history of bladder cancer
 “This may be an important biomarker for prognosis,” Theodorescu says. “With additional testing, we could use the signature to predict how aggressive a bladder cancer is likely to be. Knowing the risk can help doctors and patients make informed treatment decisions.”
“This may be an important biomarker for prognosis,” Theodorescu says. “With additional testing, we could use the signature to predict how aggressive a bladder cancer is likely to be. Knowing the risk can help doctors and patients make informed treatment decisions.”
—-
This work was supported in part by National Institutes of Health grants CA075115 and CA104106.
###
Garth Sundem
Colorado Cancer Blogs
University of Colorado Board of Regents