Health Centers > Cancer Health Center > Cancer of the Penis
Cancer of the Penis
More than 95% of penile cancers are squamous cell carcinomas (Figure 112-1). Verrucous carcinoma, known alternatively as giant condyloma or Buschke-Lowenstein tumor, is a variant of squamous carcinoma which does not metastasize, but which spreads aggressively by local extension and destroys surrounding tissues (Figure 112-2). Epidemic Kaposi's sarcoma, associated with acquired immunodeficiency syndrome (AIDS) is being increasingly encountered (Figure 112-3). Some 20% of male patients with AIDS may be expected to manifest a penile lesion in the course of the disease. Melanoma, sarcomas, and basal cell carcinoma involve the penis infrequently, but have been reported.
Bowen's disease is intraepithelial squamous carcinoma in situ. When it involves the penis, it is known as erythroplasia of Queyrat. These lesions have the potential to develop into invasive squamous carcinoma.

Paget's disease of the penis is quite rare, but may develop primarily or as the result of an underlying adenocarcinoma of the urethra or periurethral glands. Balanitis xerotica obliterans, leukoplakia, and penile cutaneous horn may occasionally develop into squamous carcinoma. Bowenoid papulosis, a reddish, raised lesion resembling erythroplasia of Queyrat, but with a benign course, may be difficult to distinguish from more problematic lesions. Biopsy is required to establish a diagnosis.
Epidemiology & Etiology
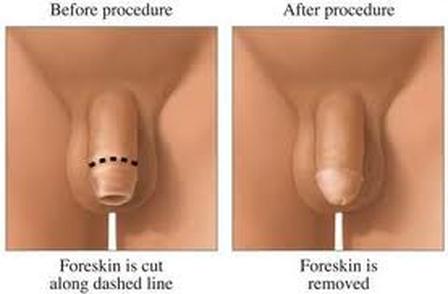
In countries where infant circumcision is common, such as Israel and the United States, the incidence of squamous carcinoma of the penis is low. Circumcision later in life does not seem to confer protection. It has been thought that chronic exposure to smegma, a substance secreted by Tyson's glands in the prepuce, might be one mechanism for the development of squamous penile cancers. In the uncircumcised penis, proper hygiene may be made more difficult by phimosis, promoting chronic inflammation of the glans and preputial tissues. With improved socioeconomic conditions, the incidence of penile cancer has fallen and the stage at presentation has also decreased, suggesting that a combination of improved education coupled with more attentive hygiene has reduced the incidence and severity of the disease.
An association between cervical cancer in women whose spouses have penile cancer has been observed, and there is evidence to suggest that patients infected with human papillomavirus (HPV) types 16, 18, 31, and 33 may have a predisposition to develop squamous carcinoma in both the penis and the cervix. Men may develop condyloma acuminata from this infection, may be totally asymptomatic carriers, or may harbor intraurethral lesions unknown to the patient which may shed the virus and expose a sexual partner.
Several large studies have dmonstrated that smoking is associated with an increased incidence of squamous cell carcinoma of the penis. Recent studies linkng smoking to high-grade lesions of the cervix and vulva suggest an association between HPV, smoking, and cancer, which may also pertain in squamous cell cancer of the penis.
Carcinoma in SITU
Erythroplasia of Queyrat (Figure 112-4) is characterized by a shiny, erythematous maculopapular patch, which is slightly raised, velvety in appearance, and typically involves the glans or prepuce. Bowen's disease appears scaly and red, is clearly demarcated, and often involves the scrotum and base of the penis. Histologically these lesions demonstrate dyskeratosis, vacuolization, and large nuclei with numerous atypical mitotic figures. The full thickness of the epithelium is involved. Clinically, erythroplasia of Queyrat and Bowen disease are the same disease, with a 10% to 20% association with progression to squamous carcinoma of the penis.
Cancer of the Penis
Histopathology
Epidemiology & Etiology
Carcinoma in SITU
Invasive Squamous Carcinoma
Verrucous Carcinoma
Other Malignancies
Natural History & Course
Tumor Staging
Surgical Treatment
Management of the Regional Lymph Nodes
Tumor Grade
Pelvic Lymphadenectomy
Radiotherapy
Chemotherapy
Prognosis
Conclusions
- Carcinoma of the Urethra
Introduction
Male Urethral Carcinoma
- Summary
- References
Invasive Squamous Carcinoma
Early invasive tumors may be small and largely unremarkable, sometimes resembling small abrasions or callused thickenings of penile skin. The initial lesion of squamous carcinoma most commonly presents on the glans or prepuce. It varies from a small, velvety, reddened, raised maculopapule to an ulcer, hyperkeratotic area, or exophytic papillary tumor (Figure 112-5). Biopsy is required to make the diagnosis, and should include contiguous normal skin for comparison.
More advanced lesions may be exophytic or ulcerated (Figure 112-6), and very advanced cancers may completely destroy the penile shaft. Metastases to the inguinal lymph nodes may produce large ulcerations in the groins late in the course of the disease. Well-differentiated tumors tend to metastasize infrequently, while more poorly differentiated tumors have a high propensity for early metastasis. Several studies confirm that higher tumor grade increases the likelihood of inguinal nodal metastases.
Verrucous Carcinoma
Verrucous carcinoma, or Buschke-Lowenstein tumor of the penis, comprises approximately 5% of all penile cancers and represents a special variant of squamous carcinoma (see Figure 112-2). It is well differentiated and does not metastasize, but spreads aggressively by local extension and may destroy penile tissues entirely if left untreated. These lesions are often associated with HPV types 6 and 11.
Other Malignancies
Rarely, transitional cell carcinomas of the bladder or urethra may extend to the glans and prepuce. Basal cell carcinoma, melanoma, and primary sarcomas are quite rare. Kaposi sarcoma, usually the epidemic or AIDS-associated variety, is becoming an increasingly common problem. Local symptomatic management is recommended, although with large tumors surgical intervention may be required. Infiltration of the penile structures with lymphoma or leukemia usually presents as priapism. A thorough search for systemic disease is always indicated. Treatment is with systemic chemotherapy.
Natural History & Course
Squamous carcinoma of the penis usually presents as a sore or ulcer of the glans, coronal sulcus, or prepuce. In the uncircumcised male, induration or swelling of the distal penis suggests tumor. Biopsy of the lesion following dorsal slit or circumcision confirms the diagnosis.
Erythroplasia of Queyrat, verrucous carcinoma, and various hyperkeratotic lesions may evolve into squamous carcinoma or may coexist with it. Prompt treatment of these lesions is indicated.
Invasive squamous carcinoma of the penis follows a predictable pattern of metastasis. Lesions of the glans, coronal sulcus, prepuce, and distal shaft spread to the deep inguinal nodes, while lesions of the proximal shaft and base of the penis spread to the more lateral and superficial inguinal nodes. Subsequent spread to the external iliac, obturator, and iliac chains follows. Although "skip" metastases to the pelvic nodes have been reported, reevaluation of old reports and more recent series suggest that pelvic metastases in the absence of inguinal metastases probably do not occur. Metastases to distant sites are infrequent and occur late in the course of the disease.
Because primary lesions may be infected or chronically inflamed, secondary inflammation of the inguinal nodes is often present which may be impossible to distinguish from metastatic disease. Careful reexamination of the inguinal nodes following a 4- to 6-week course of broad-spectrum antibiotic therapy may help to differentiate inflammation from cancer.
Tumor Staging
Once the diagnosis of squamous carcinoma is established, complete staging is undertaken. Careful palpation of the inguinal nodes is carried out. Additional staging studies should include chest radiograph, computerized tomography (CT) of the pelvis and inguinal regions, and possibly magnetic resonance scanning (MRI). In instances patients who are obese or whose groins were subjected to prior surgery, CT or MRI may be superior to palpation in detecting suspicious nodal enlargement. CT and MRI have supplanted lymphangiography as a staging procedure.
The American Joint Committee on Cancer (AJCC) TNM (Tumor, Nodes, Metastases) system of 1997 is the accepted staging system for penile cancer (Table 112-1). The older Jackson system, which is clinically based, is no longer used, but is frequently encountered in the older literature (Table 112-2).
Cancer of the Penis Surgical Treatment
Treatment of penile cancer is based on the extent of the primary tumor and its tumor grade, established by biopsy of the lesion. Antibiotic therapy is begun prior to biopsy and continued through surgical therapy and for 4 to 6 weeks afterwards. Once the tissue diagnosis is confirmed, small superficial tumors may be successfully treated with local surgical excision, topical chemotherapy, laser surgery, Mohs micrographic surgery, or superficial radiation therapy.
Larger tumors with invasion may sometimes be managed with organ-sparing surgery or radiotherapy, but deeply invasive cancers, particularly those that deform the glans or involve the shaft structures, may not be amenable to conservative measures.
Lesions which involve the distal shaft or glans are usually managed by partial penectomy, providing that a 2-cm margin can be achieved while leaving enough penile length to allow the patient to void while standing and to engage in intercourse. More advanced lesions or tumors that involve the base of the penis are best managed by total penectomy with creation of a perineal urethrostomy. More extensive lesions or those involving the base and bulbar urethral portion of the penis may require cystoprostatectomy or occasionally anterior or total pelvic exenteration, with urinary diversion.
Management of the Regional Lymph Nodes
Proper management of the inguinal and pelvic lymph nodes in patients with squamous carcinoma of the penis has been one of the most challenging and controversial aspects of penile cancer treatment. Lymphatic drainage of the penile shaft and base is to the superficial inguinal lymph nodes. Drainage from the glans, prepuce, and distal shaft is to the deep inguinal nodes. There is crossover of the lymphatic channels at the base of the penis so that a lesion on one side of the penis may metastasize to the contralateral inguinal nodes. The deep inguinal nodes drain to the external iliac and obturator chains and subsequently to the common iliac nodes and the retroperitoneal nodal tissue surrounding the aorta and inferior vena cava.
Several clinical studies in patients with inguinal metastases show that a meticulous inguinal node dissection is curative in 40% to 60% of cases. However, the traditional node dissection carries with it a high likelihood of morbidity - flap necrosis, wound infection, chronic lymphangitis, lymphocele, and chronic lower limb edema. A modified, somewhat less-extensive dissection has been adopted by most surgeons, which has reduced some of the unpleasant sequelae of groin dissection. Nonetheless, an inguinal node dissection is not undertaken lightly, and the indications for a groin dissection in patients with no palpable inguinal nodes are not clear. While approximately 25% of patients with impalpable nodes will have metastatic disease and must undergo a node dissection, other patients with no metastases undergo needless surgery. Determining which patients should have inguinal lymphadenectomy and which may be followed expectantly is a major challenge in the management of this disease. Patients with metastases to the groins who do not undergo appropriate node dissection usually die of their disease within 3 years.
Clinical staging of the inguinal nodes is highly inaccurate. Several studies demonstrate that microscopic metastases may be present in impalpable nodes, while palpably enlarged nodes are benign half of the time. Staging techniques using lymphangiography with aspiration of the nodes are unsatisfactory. The sentinel node biopsy, proposed by Cabanas and associates, while initially encouraging, is also unreliable and has been abandoned. Patients with negative sentinel nodes have developed inguinal metastases after negative bilateral sentinel node biopsies.
Tumor Grade
Recent studies confirm the importance of tumor grade as well as stage in assessing the risk of nodal metastases, and help to clarify when node dissection should be performed. Patients with grade I tumors, which are limited to the skin and superficial tissues of the penis, are unlikely to have spread to inguinal nodes. Patients with grade II or grade III lesions with any degree of invasion of the deeper penile structures are at significant risk of groin metastases. While for many years patients with clinically negative inguinal nodes were followed expectantly and subjected to inguinal node dissection only if palpable node metastases developed, contemporary investigators recommend early surgery if high-grade tumor (grade II or III) and more than superficial invasion is documented on biopsy. Physicians at my institution treat patients with 4 to 6 weeks of broad-spectrum antibiotic therapy and then perform a modified bilateral inguinal node dissection on any patient with palpably enlarged inguinal nodes, and on patients with impalpable nodes who demonstrate invasion into the penile shaft or show grade II or grade III histopathology on their biopsy.
Pelvic Lymphadenectomy
Patients found to have inguinal node metastases should undergo pelvic lymphadenectomy on the affected side. This can be done extraperitoneally via a midline incision or through a modified Gibson or groin incision. At my institution, pelvic lymphadenectomy is done at the same time that inguinal node dissection is performed, although at some centers the procedure is staged several weeks later. Patients found to have up to three metastatic pelvic nodes, with all nodes below the bifurcation of the internal and external iliac vessels, often fare well. Metastases above the bifurcation have been almost uniformly lethal.
Radiotherapy
Primary radiotherapy of penile cancer is used more widely in Europe than in the United States. It may be appropriate in small superficial lesions or in selected larger lesions when organ preservation is the goal and when patients refuse surgery. In more advanced lesions, however, tissue preservation may not be feasible. Concurrent chemotherapy may enhance the effectiveness of radiation.
Radiotherapy may be administered as teletherapy using cobalt or linear accelerators, or as brachytherapy, with a mold or with iridium192 wires. Iridium192 or cesium137 may be used to boost dosages in bulky or extremely cornified tumors. Normally doses of 30 to 50 Gy given over 3 to 5 weeks are used. Boosts to 65 to 70 Gy using various brachytherapy techniques may follow if clinically indicated. Radiation is often the treatment of choice in symptomatic lesions resulting from epidemic (AIDS-related) Kaposi's sarcoma.
Acute radiation reactions - edema and tissue inflammation, with concomitant skin irritation, tenderness, and dysuria - are common accompaniments of both external radiation and brachytherapy. Such symptoms usually recede promptly once therapy is completed. Long-term effects of treatment may include telangiectasia, hyperpigmentation, diminished sensation, scarring, and atrophy of the treated tissues. Fibrotic change and fistulization may occur in large lesions where significant tissue damage has occurred prior to radiotherapy. Late recurrences in radiated sites may occur up to a decade following definitive treatment, so close follow-up is essential.
Radiation of clinically negative groins as a prophylactic measure is controversial as is adjuvant radiation to the groins following inguinal surgery. While some studies suggest a benefit from such treatment, others show no improvement when compared with patients treated with surgery alone.
Cancer of the Penis - Chemotherapy
Chemotherapy is used as an adjuvant to definitive surgical or radiation therapy or occasionally as a radiopotentiator. Experience is limited by the relative rarity of the disease. Multidrug combination chemotherapy programs have shown promise at several institutions. Pizzocaro and Piva of the Milan National Tumor Institute have used combination chemotherapy with vincristine, bleomycin, and methotrexate (VBM) in patients with fixed nodal metastases, and have been successful at rendering them resectable. Dexeus and associates from M.D. Anderson Cancer Center have used cisplatin-based chemotherapy as adjuvant therapy following surgery. Similarly, a recently completed multiinstitutional Southwest Oncology Group trial using methotrexate, cisplatin, and bleomycin to treat advanced, unresectable inguinal metastatic disease demonstrated a 32.5% response rate, although toxicity was high. Several combination chemotherapy protocols, which have shown effectiveness in treating squamous carcinoma of other sites - anus, esophagus, head and neck - remain to be tested in squamous carcinoma of the penis. Multiinstitutional, multinational trials are required to enroll sufficient numbers of patients to provide meaningful data.
Cancer of the Penis Prognosis
Left untreated, squamous carcinoma of the penis is invariably lethal, killing most of those afflicted within 3 years. Outcome is directly related to the extent of the disease at diagnosis and the presence or absence of inguinal metastases.
The national Surveillance, Epidemiology, and End Results (SEER) database (1973 to 1987; 1,101 patients) shows a relative survival rate of 95% for patients with carcinoma in situ and 70% for all stages. Relative 5-year survival for localized tumor was 80%, with survival rates of 52% for regional (nodal) disease and 18% for distant disease. Horenblas and associates reported 93% 5-year survival when nodes were negative, versus 50% in patients with clinically positive nodes. Srinivas and associates reported a crude 5-year survival rate of 28% in patients with proven inguinal metastases. Patients with minimal nodal disease (N1,N2) had 5-year survivals of 50% to 80%, while those with N3 or N4 disease had a much graver outcome, with survivals of 4% to 12%. Patients with negative groins had a 74%, 5-year survival. The outcome of patients with pelvic metastases has been very poor.
Conclusions
Squamous carcinoma of the penis is a largely preventable disease; in fact, incidence has fallen over the past two decades with improved socioeconomic conditions and access to health care. Better understanding of the importance of tumor histology and a more aggressive approach to inguinal disease may provide further improvements in survival. Refinements in surgical and radiotherapeutic techniques have further improved outcome and quality of life. Early recognition of tumor lesions has allowed for effective but less-extensive treatment and improvements in organ-sparing procedures.
Further research into combined modality therapies using chemotherapy in conjunction with surgery, radiation therapy, or both will likely further improve treatment results. Improved understanding of the role of possible causative agents (HPVs and human herpesviruses) should improve both treatment and prevention.