Health Centers > Cancer Health Center > Salivary Gland Tumors
Salivary Gland Tumors
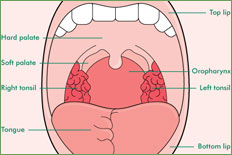
The paired major salivary glands consist of the parotid and submandibular glands. Minor salivary glands are widely distributed in the mucosa of the lips, cheeks, hard and soft palate, uvula, floor of mouth, tongue, and peritonsillar region; a few are found in the nasopharynx, paranasal sinuses, larynx, trachea, bronchi, and lacrimal glands.
Salivary Gland Tumors (patient information)
Anatomy
Pathology
Diagnosis
Treatment
Prognosis
References
Salivary Gland Tumors (for professionals)
Anatomy
Diagnosis
Histopathology
Staging
Prognosis
Neutron Radiotherapy
Chemotherapy
Pathology
A variety of site-specific and systemic diseases can affect the salivary glands. Tumors of salivary gland tissue constitute about 5% of head and neck tumors and affect major salivary glands five times more often than minor salivary glands. The incidence of malignancy among salivary gland tumors varies inversely with the size of the gland. About 15% of parotid tumors, 50% of submandibular gland tumors, and 90% of minor salivary gland tumors are malignant.
Since 70% of salivary gland tumors occur in the parotid and 85% of these are benign, the majority of salivary gland tumors are benign. These tumors are thought to originate from two cell types: intercalated and excretory duct cells. Myoepithelial cells are present in many salivary gland tumors but rarely present as the principal cell type. The differential diagnosis of a swelling in the parotid region includes parotitis, a primary parotid tumor, upper jugular chain lymph node enlargement, a tumor of the tail of the submandibular gland, an enlarged preauricular or parotid lymph node, a branchial cleft cyst, an epithelial inclusion cyst, or a mesenchymal tumor.
The most common benign salivary gland tumor is the benign mixed tumor or pleomorphic adenoma, which accounts for 70% of parotid tumors and 50% of all salivary gland tumors. Mixed tumors are more common in women than in men, with the peak incidence in the fifth decade. They are slow-growing and lobular and may become very large without interfering with facial nerve function. Although mixed tumors are benign, they will recur after surgery unless they are completely removed. Enucleation is inadequate surgery. When tumor recurs in the parotid region, the facial nerve is at greater risk from damage during reoperation than it was during the initial procedure. Malignant transformation in a benign tumor is uncommon but can occur (malignant mixed carcinoma).
Warthin's tumor (papillary cystadenoma lymphomatosum), the next most common benign tumor, accounts for about 5% of parotid tumors. Warthin's tumors are usually cystic, typically occur in men in the sixth and seventh decades, and are bilateral in about 10% of cases. They occur almost exclusively in the parotid gland and have a typical histologic appearance, consisting of a papillary-cystic pattern with a marked lymphoid component. Oncocytomas are benign tumors composed of large oxyphilic cells called oncocytes. On electron microscopy, the cytoplasm of the oxyphilic cells is packed with mitochondria. Monomorphic tumors are rare benign salivary gland tumors that are usually epithelial but occasionally myoepithelial in origin. They are most commonly seen in the minor salivary glands of the lip.
Mucoepidermoid carcinoma is the most common parotid cancer. These tumors are categorized as high-grade, intermediate-grade, or low-grade cancers. Acinic cell cancers are derived from serous acinar cells and are found almost exclusively in the parotid gland. Adenoid cystic carcinomas, which are uncommon in the parotid, have a great propensity for perineural invasion and local recurrence. Patients with this cancer tend to have protracted illness, with recurrences appearing 15 years or more after treatment. Patients with distant metastases from adenoid cystic carcinoma can survive for 5 or more years. Less common cancers include cancer arising in a mixed tumor and primary squamous cancer, which accounts for approximately 1% of salivary gland cancers and must be differentiated from mucoepidermoid carcinoma and metastatic squamous carcinoma in a parotid lymph node. Among minor salivary gland cancers, adenoid cystic carcinoma is the most common cancer, followed by adenocarcinoma and mucoepidermoid carcinoma. Approximately 70% of all minor salivary gland cancers occur in the oral cavity, principally on the hard palate.
Diagnosis
Cancer of the Nasal Cavity, Napopharynx, and Paranasal Sinuses
Anatomy
Pathology
Clinical Findings
Diagnosis
Treatment
Prognosis
References
In most cases, local excision with a margin of normal tissue is the appropriate form of biopsy for a major salivary gland tumor. In the parotid region, this requires identification of the facial nerve. For submandibular tumors, the entire submandibular triangle is cleared. In contrast, minor salivary gland tumors have a higher likelihood of being malignant, and an incisional biopsy is performed initially so that definitive treatment can be planned. In the parotid region, the presence of pain, recent rapid enlargement of a preexisting nodule, skin involvement, or facial nerve paralysis suggests cancer. Enlarged cervical lymph nodes in association with a salivary gland tumor are considered a manifestation of cancer until proved otherwise. Fine-needle aspiration is indicated if accurate diagnosis will allow for better treatment planning.
T STAGE: MAJOR SALIVARY GLAND CANCER
T1 Tumor 2 cm or less in greatest dimension without invasion of surrounding soft tissues T2 Tumor more than 2 cm but not more than 4 cm in greatest dimension without invasion of surrounding soft tissues T3 Tumor more than 4 cm in size and/or invading into surrounding soft tissues T4 Tumor invades skin, mandible, ear canal and/or facial nerve
Treatment
Benign salivary gland tumors are excised. Parotid surgery requires a preauricular incision carried onto the neck to allow adequate exposure of the gland and facial nerve. The aim of the operation is to completely excise the tumor with an adequate margin of normal tissue. Enucleation is avoided because it greatly increases the likelihood of recurrence and nerve damage. When a tumor arises in the parotid gland deep to the facial nerve, the portion of the parotid gland superficial to the facial nerve is removed, the facial nerve is then elevated, and finally the tumor deep to the nerve is removed along with the remaining parotid tissue. Benign tumors of the submandibular gland require total removal of the gland for diagnosis and treatment.
Cancer of the Oral Cavity
Anatomy
Pathology
Clinical Findings
Treatment
¬ Primary Cancer
¬ Management of Neck Metastases
Prognosis
Surgical treatment for parotid cancer depends on the extent of the cancer. Unless the facial nerve is paralyzed or found to be directly invaded by cancer at surgery, it is preserved. When the facial nerve must be divided, it is repaired if it was functioning normally prior to surgery. The facial nerve can be reconstructed using a nerve graft, eg, the greater auricular or sural nerves. Recovery of function can take many months and is often incomplete.
For low-grade salivary gland cancers, complete excision is sufficient treatment. For high-grade cancers, postoperative radiation therapy is indicated for the primary cancer site and regional lymph nodes. Clinically involved lymph nodes are removed by a radical or modified neck dissection. Elective neck dissections are generally not indicated, though removal of level II cervical lymph nodes requires minimal additional surgery after parotidectomy or after removal of the contents of the submandibular triangle.
The majority of salivary gland tumors arise in the parotid glands, and although 80% of these are benign, these glands are the origin of the majority of malignant tumors. Tumors arising in the submandibular, sublingual, or minor salivary glands are more likely to be malignant.
The largest salivary glands are the parotids, which are located on the cheeks anterior to the external auditory canal and pinna. The gland wraps around the mandible, and as the facial nerve passes through the parotid, it divides it into superficial or lateral and deep lobes. About 80% of the gland lies lateral to the facial nerve, and 20% lies deep to this nerve and behind and medial to the mandible. The internal carotid artery, the internal jugular vein, the cervical sympathetic chain, and cranial nerves IX, X, and XI are in close proximity to the deep lobe of the parotid » »
Prognosis
The prognosis for salivary gland cancer depends on the stage, the histologic grade, the cancer site, the patient's age, and the adequacy of surgical removal. The most important prognostic factor is the cancer stage. The next most important factor is the histologic grade of the cancer. Low-grade cancers such as acinic cell cancers and low-grade mucoepidermoid cancers usually present as stage I or stage II cancers and have an excellent prognosis, with 10-year survival rates of about 80%. On the other hand, the 10-year survival rate after treatment of high-grade stage III and stage IV cancers-such as-adenocarcinoma, squamous cell carcinoma, and high-grade mucoepidermoid carcinoma-is about 30%.
References
Douglas JG et al: Gamma knife stereotactic radiosurgical boost for patients treated primarily with neutron radiotherapy for salivary gland neoplasms. Stereotact Funct Neurosurg 2004;82:84. Pubmed: 15305080
Douglas JG et al: Treatment of salivary gland neoplasms with fast neutron radiotherapy. Arch Otolaryngol Head Neck Surg 2003;129:944. Pubmed: 12975266
Spiro JF et al: Cancer of the parotid gland: Role of 7th nerve preservation. World J Surg 2003;27:863. Pubmed: 14509520