Health Centers > Cancer Health Center > Germ Cell Tumors of the Testis
Germ Cell Tumors of the Testis
Malignant tumors of the testis are rare, with approximately 2-3 new cases per 100,000 males reported in the United States each year. Of all primary testicular tumors, 90-95% are germ cell tumors (seminoma and nonseminoma), while the remainder are nongerminal neoplasms (Leydig cell, Sertoli cell, gonadoblastoma). The lifetime probability of developing testicular cancer is 0.2% for a white male in the United States. Survival of patients with testicular cancer has improved dramatically in recent years, reflecting the development and refinement of effective combination chemotherapy. Overall 5-year survival rates have increased from 78% in 1974-1976 to 91% in 1980-1985 (P < .05).
The incidence of testicular cancer shows marked variation among different countries, races, and socioeconomic classes. Scandinavian countries report up to 6.7 new cases per 100,000 males annually; Japan reports 0.8 per 100,000 males. In the United States, the incidence of testicular cancer in blacks is approximately one-fourth that in whites. Within a given race, individuals in the higher socioeconomic classes have approximately twice the incidence of those in the lower classes.
Testicular cancer is slightly more common on the right side than on the left, which parallels the increased incidence of cryptorchidism on the right side. Of primary testicular tumors, 1-2% are bilateral, and about 50% of these tumors occur in men with a history of unilateral or bilateral cryptorchidism. Primary bilateral tumors of the testis may happen synchronously or asynchronously but tend to be of the same histologic type. Seminoma is the most common germ cell tumor in bilateral primary testicular tumors, while malignant lymphoma is the most common bilateral tumor of the testis.
Although the cause of testicular cancer is unknown, both congenital and acquired factors have been associated with tumor development. The strongest association has been with the cryptorchid testis. Approximately 7-10% of testicular tumors develop in patients who have a history of cryptorchidism; seminoma is the most common form of tumor these patients have. However, 5-10% of testicular tumors occur in the contralateral, normally descended testis. The relative risk of malignancy is highest for the intra-abdominal testis (1 in 20) and is significantly lower for the inguinal testis (1 in 80). Placement of the cryptorchid testis into the scrotum (orchiopexy) does not alter the malignant potential of the cryptorchid testis; however, it does facilitate examination and tumor detection.
Exogenous estrogen administration to the mother during pregnancy has been associated with an increased relative risk for testicular tumors in the fetus, ranging from 2.8 to 5.3 over the expected incidence. Other acquired factors such as trauma and infection-related testicular atrophy have been associated with testicular tumors; however, a causal relationship has not been established.
There are two main types of testicular germ cell tumours:
- Seminomas- this type of tumour generally occurs in men between the ages of 25 and 55.
- Nonseminomas- Unlike seminomas, nonseminomas tend to grow and spread at a faster rate.
Teratomas are one type of nonseminoma. They can be either benign or malignant. Unlike other germ cell tumours they are not as sensitive to chemotherapy and therefore their main treatment is surgery.
Teratomas usually occur in men between the ages of 15 and 35.
Germ cell tumours can also occur in children and can found in other parts of the body including the abdomen, chest and brain.
What causes a testicular germ cell tumour?
The exact causes of testicular germ cell tumours are unknown. However, there are a few factors that increase the risk:
- Failed testicular descent: failure of the testes to descend into the scrotal sac (normally the testicles descend in the first year of a baby's life).
- Having a family history of testicular germ cell tumours.
- Background- testicular germ cell tumours are more common in white men than African-Caribbean or Asian men.
What are the symptoms?
Some of the symptoms of a testicular germ cell tumour may include:
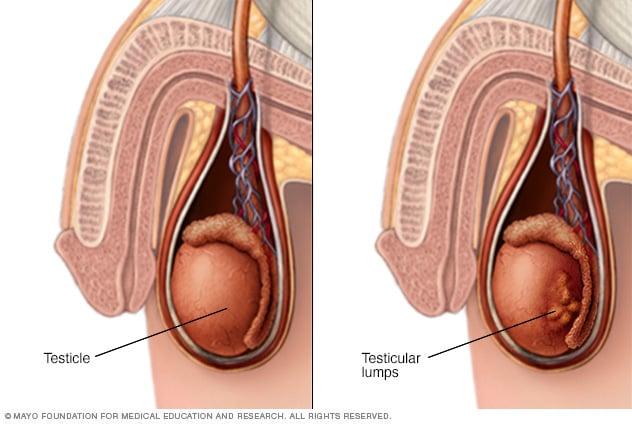
- A painless lump in the testicle
- Swelling
- Pain or discomfort in a testicle or in the scrotum
- Ache in the groin or abdomen
- Heavy feeling in scrotum
- Rarely, tender nipples may be caused by hormonal changes within the body.
Self Examination
Although testicular germ cell tumours do not always produce early symptoms, self examination is recommended for people who are at a higher risk of developing a testicular germ cell tumour.
The best time to do this is after a warm bath or shower, when the scrotal skin is relaxed. Click here for more information and tips on how to conduct a testicular self-examination.
How is it diagnosed?
After visiting a GP a referral will probably be made to a hospital for some tests.
Firstly they will complete a physical examination followed by an ultrasound of the testicles to detect any abnormalities.
If these tests detect a possible testicular germ cell tumour further tests may include:
- Blood Tests- this can help to determine the exact type of tumour and at what stage the tumour is at.
- X-ray
- CT Scan
- MRI
- Biopsy
- Radical Orchiectomy- sometimes the removal of a testicle is required for further testing.
If the results of the test show testicular cancer, another referral will be made to a doctor who specialises in the treatment of the reproductive organs.
Staging
The stage of a cancer describes its size and whether it has spread beyond the area of the body where it started. A staging system commonly used is called the TNM system. It is described here:
- T: refers to the tumour size.
- N: refers to whether lymph nodes are affected.
- M: refers to whether cancer has spread to other parts of the body (metastases).