Health Centers > Cancer Health Center > Non-Germ Cell Tumors of the Testis
Non-Germ Cell Tumors of the Testis
Approximately 5-6% of all testis tumors are non-germ cell tumors of the testis. Three types will be considered, namely, Leydig cell tumors, Sertoli cell tumors, and gonadoblastomas.
1. Leydig Cell Tumors
Epidemiology & Pathology
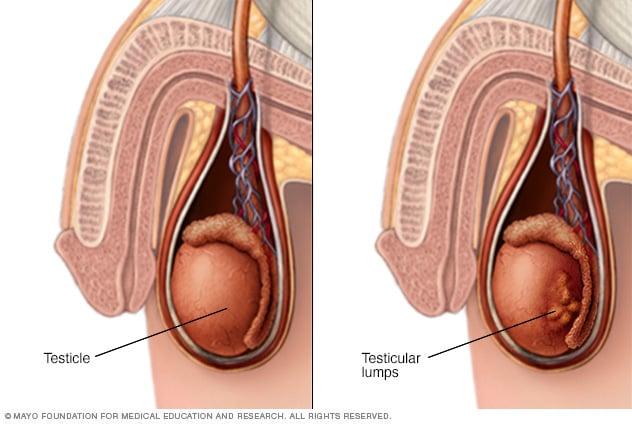
Leydig cell tumors are the most common non-germ cell tumors of the testis and account for 1-3% of all testicular tumors. They follow a bimodal age distribution: the 5- to 9-year-old and the 25- to 35-year-old age groups. Twenty-five percent of these tumors occur in childhood. Bilaterality is seen in 5-10% of cases. The cause of these tumors is unknown; unlike germ cell tumors, there is no association with cryptorchidism.
Pathologic examination reveals a small, yellow, well-circumscribed lesion devoid of hemorrhage or necrosis. Microscopically, hexagonally shaped cells with granular, eosinophilic cytoplasm containing lipid vacuoles are seen. Reinke crystals are fusiform-shaped cytoplasmic inclusions that are pathognomonic for Leydig cells.
Clinical Findings
Prepubertal children usually present with virilization, and tumors are benign. Adults are usually asymptomatic, although gynecomastia may be present in 20-25%. Ten percent of tumors in adults are malignant. Laboratory findings include elevated serum and urinary 17-ketosteroids as well as estrogens.
Treatment & Prognosis
Radical orchiectomy is the initial treatment for Leydig cell tumors. Clinical staging is similar to that for germ cell tumors, and levels of the 17-ketosteroids can be helpful in distinguishing between benign and malignant lesions. Elevations of 10-30 times normal are typical of malignancy. RPLND is recommended for malignant lesions. Because of the rarity of these lesions, the role of chemotherapy remains to be defined. Prognosis is excellent for benign lesions, while it remains poor for patients with disseminated disease.
2. Sertoli Cell Tumors
Epidemiology & Pathology
Sertoli cell tumors are exceedingly rare, composing less than 1% of all testicular tumors. A bimodal age distribution is seen: 1 year old or younger and the 20- to 45-year-old age group. Approximately 10% of the lesions are malignant. Gross examination reveals a yellow or gray-white lesion with cystic components. Benign lesions are well circumscribed, while malignant lesions show ill-defined borders. Microscopically, tumors appear heterogeneous with mixed amounts of epithelial and stromal components. Sertoli cells are columnar or hexagonal cells with a large nucleus and solitary nucleolus and contain vacuolated cytoplasm.
Clinical Findings
A testicular mass is the most common presentation. Virilization is often seen in children, and gynecomastia may be present in 30% of adults. Because of the rarity of these tumors, minimal endocrine data are available on these patients.
Treatment Radical orchiectomy is the initial procedure of choice. In cases of malignancy, RPLND is indicated; however, the roles of chemotherapy and radiotherapy remain unclear.
3. Gonadoblastomas
Epidemiology & Pathology
Gonadoblastomas comprise 0.5% of all testicular tumors and are almost exclusively seen in patients with some form of gonadal dysgenesis. Most of these tumors occur in patients under 30 years of age, although the age distribution ranges from infancy to beyond 70 years.
Gross examination reveals a yellow or gray-white lesion that can vary in size from microscopic to greater than 20 cm and may exhibit calcifications. Microscopically, 3 cell types are seen: Sertoli cells, interstitial cells, and germ cells.
Clinical Findings
The clinical manifestations are predominantly related to the underlying gonadal dysgenesis and are discussed elsewhere in this book. It is noteworthy that four-fifths of patients with gonadoblastomas are phenotypic females. Males typically have cryptorchidism or hypospadias.
Treatment & Prognosis
Radical orchiectomy is the primary treatment of choice. In the presence of gonadal dysgenesis, a contralateral gonadectomy is recommended because the tumor tends to be bilateral in 50% of cases in this setting. Prognosis is excellent.