Health Centers > Cancer Health Center > Tumors of the Testis
Tumors of the Testis
Germ cell tumors of the testis are the most common cancer in young men between the ages of 15 and 35 years. Before 1970, the young man with recurrent testicular cancer following orchiectomy was destined to have rapid progression and death from disseminated disease. With the development of sophisticated high-voltage radiation therapy technology and the application of aggressive multiagent chemotherapy since the early 1970s, this cancer is routinely cured in young men entering the most productive phase of life. Consequently, the internist caring for the testicular cancer patient in whom durable remission and long-term survival are anticipated must recognize the impact of the disease and its therapy on fertility, employability, insurability, and delayed morbidity. In 1997, an estimated 7200 new cases of testis cancer will be diagnosed, yet only 350 deaths from the disease are expected. Testicular cancer is infrequent, occurring with an incidence of approximately 2 per 100,000 males. The incidence has been rising in white males while remaining stable in black males.
Relevant Physiology and Pathophysiology
The major risk factors for the development of testis cancer are male gender and cryptorchidism. However, maldescent of the testis does not seem to be causal in the development of testicular cancer but rather a marker for some genetic or dysgenic event in embryonic or fetal life. The opposite normally descended testis develops cancer in about one quarter of cryptorchid testis cancer patients. Orchiopexy fails to restore normal cancer risk to the patient with testicular maldescent, but it does allow adequate examination of the testis for development of cancer. Other risk factors include various genitourinary abnormalities such as inguinal hernia, ureteral duplication, abnormal lobulation or orientation of the kidney, and testicular hydroceles.
Germ cell tumors of the testis represent greater than 90% of all tumors of the testis. These tumors appear to arise from a pluripotent germ cell capable of differentiating into embryonic structures (teratoma and embryonal carcinoma), placental structures (yolk-sac tumor and choriocarcinoma) or seminoma (the most primitive germ cell tumor). Germ cell cancers may express features of only one of these histopathologies or mixtures of two or more. Other malignancies of the testis include lymphoma (the most common non-germ cell cause of testicular malignancy in elderly men), metastatic cancer or leukemia, tumors of the testicular stroma, and other rare tumors.
Laboratory and Other Diagnostic Tests
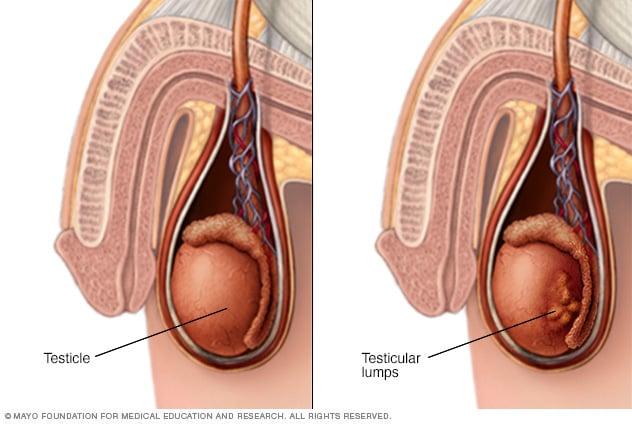
The diagnosis of germ cell tumor of the testis requires histopathologic examination of tissue obtained from an orchiectomy specimen. Inguinal orchiectomy, rather than transcrotal biopsy, is the preferred surgical approach for retrieval of diagnostic testicular tissue. The risk of contamination of the scrotal skin followed by local recurrence of cancer or risk of distribution of microscopic metastases to inguinal lymphatic drainage is circumvented. Because the tumor may contain histologic mixtures of several germ cell elements, it is essential that a total orchiectomy specimen plus a generous margin of spermatic cord be provided the pathologist. Occasionally extragonadal germ cell tumors may present within the mediastinum or retroperitoneum without an identifiable testicular tumor. A major proportion of patients with these unusual malignancies may expect cure with systemic chemotherapy. As a consequence, representative incisional biopsy rather than wholesale excision of these frequently bulky tumors is sufficient to guide therapeutic recommendations. Ultrasonography of the testes should be performed in the event that there is doubt about which testis may harbor the tumor, that bilateral tumors are suspected, or that there is an extragonadal presentation of a germ cell tumor.
The availability of sensitive serum assays for α fetoprotein (AFP) and for the β-subunit of human chorionic gonadotropin (β-HCG) has markedly enhanced the accurate and aggressive management of patients with germ cell tumors. AFP is produced by embryonal carcinoma, yolk sac, and occasionally teratomatous components of germ cell tumors. The half-life of this glycoprotein is 5 to 7 days. β-HCG is produced by syncytiotrophoblastic cells found in seminoma, choriocarcinoma, and embryonal carcinomas.
Germ Cell Tumors of the Testis
- Epidemiology & Risk Factors
- Classification
- Tumorigenic Hypothesis for Germ Cell Tumor Development
- Pathology
- Patterns of Metastatic Spread
- Clinical Staging
- Clinical Findings
- Differential Diagnosis
- Treatment
- Follow-up Care
- Prognosis
Non-Germ Cell Tumors of the Testis
- Leydig Cell Tumors
# Epidemiology & Pathology
# Clinical Findings
# Treatment & Prognosis
- Sertoli Cell Tumors
# Epidemiology & Pathology
# Clinical Findings
# Treatment
- Gonadoblastomas
# Epidemiology & Pathology
# Clinical Findings
# Treatment & Prognosis
Secondary Tumors of the Testis
- Lymphoma
# Epidemiology & Pathology
# Clinical Findings
# Treatment & Prognosis
- Leukemic Infiltration Of the Testis
- Metastatic Tumors
Extragonadal Germ Cell Tumors
Tumors of the Penis
- Epidemiology & Risk Factors
- Pathology
- Patterns of Spread
- Tumor Staging
- Clinical Findings
- Differential Diagnosis
- Treatment
- Prognosis
- Other Penile Tumors