Health Centers > Cancer Health Center > Ureteral & Renal Pelvic Cancers
Ureteral & Renal Pelvic Cancers
Incidence
Carcinomas of the renal pelvis and ureter are rare, accounting for only 4% of all urothelial cancers. The ratio of bladder-renal pelvic-ureteral carcinomas is approximately 51:3:1 (Williams and Mitchell, 1973). The mean age at diagnosis is 65 years, and the male-female ratio is 2-4:1 (Babaian and Johnson, 1980; Hawtrey, 1971). Urothelial cancer often presents as a widespread urothelial abnormality: Patients with a single upper-tract carcinoma are at risk of developing bladder carcinomas (30-50%) and contralateral upper-tract carcinoma (2-4%). Conversely, patients with primary bladder cancer are at low risk (< 2%) of developing upper urinary tract cancers (Oldbring et al, 1989). However, patients with multiple, recurrent superficial and in situ bladder cancers that are successfully treated by transurethral resection and BCG are at a substantial, lifelong risk of development of upper-tract cancers (Herr, 1998). The cumulative risks of such cancers have been estimated to be 10% at 5 years of follow-up, 26% at 5-10 years, and 34% at > 10 years.
Etiology
As with bladder carcinoma, smoking and exposure to certain industrial dyes or solvents are associated with an increased risk of upper urinary tract transitional cell carcinomas (Shinka et al, 1988). However, these tumors also occur with increased frequency in patients with a long history of excessive analgesic intake, those with Balkan nephropathy, and those exposed to Thorotrast, a contrast agent previously used for retrograde pyelography. Patients with carcinomas associated with analgesic abuse are more likely to be women, have higher-stage disease, and be younger than others (Taylor, 1972; Mahoney et al, 1977). All the major constituents of the analgesic compounds consumed (acetaminophen, aspirin, caffeine, and phenacetin) may be associated with an increased risk of upper urinary tract cancer (Ross et al, 1989; Jensen et al, 1989). Balkan nephropathy is an interstitial inflammatory disease of the kidneys that affects Yugoslavians, Rumanians, Bulgarians, and Greeks (Markovic, 1972); associated upper-tract carcinomas are generally superficial and more likely to be bilateral. The exact mechanism of tumor induction in these patients remains unknown.
Pathology
The mucosal lining of the renal pelvis and ureter is similar to that of the urinary bladder, being composed of transitional cell epithelium. Thus, most renal pelvic and ureteral cancers (90% and 97%, respectively) are transitional cell carcinomas. Grading is similar to that for bladder carcinomas. Papillomas account for approximately 15-20% of cases (Grabstald, Whitmore, and Melamed, 1971; Bennington and Beckwith, 1975). They are isolated in just over 50% of patients and multiple in the rest, and in approximately 25% of patients with isolated papillomas and 50% of patients with multiple papillomas, carcinomas eventually develop. Among patients with carcinomas of the ureter, multicentricity approaches 50% (Bennington and Beckwith, 1975). There is a relationship between tumor grade and the likelihood of urothelial abnormalities elsewhere: Low-grade cancers are associated with a low incidence of urothelial atypia or CIS in remote sites; however, these abnormalities are common with high-grade neoplasms (McCarron, Chasko, and Bray, 1982). Most upper urinary tract transitional cell carcinomas are localized at the time of diagnosis; the most common metastatic sites include regional lymph nodes, bone, and lung (Abeshouse, 1956).
Squamous carcinomas account for approximately 10% of renal pelvic cancers and are much rarer in the ureter. Most carcinomas are usually sessile and infiltrating at the time of diagnosis. Such tumors are commonly identified in patients with a history of chronic inflammation from infection or calculous disease. Adenocarcinomas are very rare tumors of the upper urinary tract and, like squamous carcinomas, tend to be far advanced at the time of diagnosis.
Ureteral & Renal Pelvic Cancers
Incidence
Etiology
Pathology
Staging & Natural History
Clinical Findings
- Symptoms and Signs
- Laboratory Findings
- Imaging
- Ureteropyeloscopy
Treatment
- Future Directions
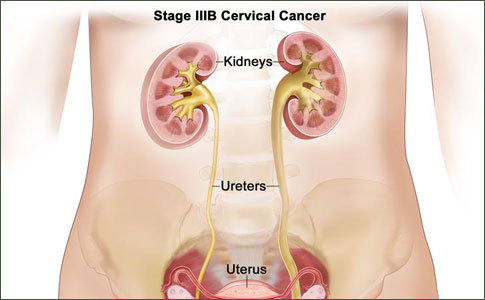
Mesodermal tumors of the renal pelvis and ureter are quite rare. Benign tumors include fibroepithelial polyps (the most common), leiomyomas, and angiomas. Fibroepithelial polyps occur most commonly in young adults and are characterized radiographically by a long, slender, and polyploid filling defect within the collecting system. The most common malignant mesodermal tumors are leiomyosarcomas. The ureter and renal pelvis may be invaded by cancers of contiguous structures, such as primary renal, ovarian, or cervical carcinomas. True metastases to the ureter are rare. The most common metastatic tumors include those of stomach, prostate, kidney, and breast as well as lymphomas (Bennington and Beckwith, 1975).
Staging & Natural History
Staging of both renal pelvic and ureteral carcinomas (Table 20-4) is based on an accurate assessment of the degree of tumor infiltration and parallels the staging system developed for bladder cancer (Batata et al, 1975; Grabstald, Whitmore, and Melamed, 1971; American Joint Committee on Cancer, 1997). Tumor stage and grade correlate with survival (Cummings et al, 1975; Batata et al, 1975; Batata and Grabstald, 1976; Bloom, Vidone, and Lytton, 1970; Reitelman et al, 1987). Low-grade and low-stage cancers of the renal pelvis and ureter are associated with survival rates between 60% and 90%, compared with 0% and 33% for tumors of higher grade or those that have penetrated deep into or through the renal pelvic or ureteral wall (Hall et al, 1998). The latter figures reflect a high likelihood of regional or distant metastases - 40% and 75% in patients with stages B and C (T2-T4) cancers, respectively.
Clinical Findings
Gross hematuria is noted in 70-90% of patients. Flank pain, present in 8-50%, is the result of ureteral obstruction from blood clots or tumor fragments, renal pelvic or ureteral obstruction by the tumor itself, or regional invasion by the tumor. Irritative voiding symptoms are present in approximately 5-10% of patients. Constitutional symptoms of anorexia, weight loss, and lethargy are uncommon and are usually associated with metastatic disease. A flank mass owing to hydronephrosis or a large tumor is detected in approximately 10-20% (Geerdsen, 1979), and flank tenderness may be elicited as well. Supraclavicular or inguinal adenopathy or hepatomegaly may be identified in a small percentage of patients with metastatic disease.
Hematuria is identified in most patients but may be intermittent. Elevated liver function levels due to liver metastases are noted in a few patients. Pyuria and bacteriuria may be identified in patients with concomitant urinary tract infection from obstruction and urinary stasis.
As with bladder cancers, upper urinary tract cancers may be identified by examining exfoliated cells in the urinary sediment. In addition, specimens may be obtained directly with a ureteral catheter or by passing a small brush through the lumen of an open-ended catheter (Gill, Lu, and Thomsen, 1973; Blute, Gittes, and Gittes, 1981; Dodd et al, 1997). Detection depends on the grade of the tumor and the adequacy of the specimen obtained: 20-30% of low-grade cancers may be detected by cytologic testing compared with more than 60% of higher-grade lesions (McCarron, Mullis, and Vaughn, 1983); using barbotage or a ureteral brush increases diagnostic accuracy (Zincke et al, 1976). The utility of the newer voided markers, such as the BTA stat test (Bard Diagnostic Sciences, Inc, Redmond, WA), in detecting upper-tract urothelial cancers has not yet been determined (Zimmerman et al, 1998).
Findings on intravenous urography in patients with upper urinary tract cancers are usually abnormal. The most common abnormalities identified include an intraluminal filling defect, unilateral nonvisualization of the collecting system, and hydronephrosis (Williams and Mitchell, 1973; Batata et al, 1975; Almgard, Freedman, and Ljungqvist, 1973). Ureteral and renal pelvic tumors must be differentiated from nonopaque calculi, blood clots, papillary necrosis, and inflammatory lesions such as ureteritis cystica, fungus infections, or tuberculosis. The intravenous urography is often indeterminate, requiring retrograde pyelography for more accurate visualization of collecting-system abnormalities and simultaneous collection of cytologic specimens. Contrast material is injected into the ureteral orifice with a bulb or acorn-tip catheter. Intraluminal filling defects may then be identified in the ureter or renal pelvis (Figure 20-5). Ureteral tumors are often characterized by dilation of the ureter distal to the lesion, creating the appearance of a "goblet." Nonopaque ureteral calculi appear as a narrowing of the ureter distal to the calculus. A ureteral catheter passed up the ureter may coil distal to a ureteral tumor (Bergman's sign) (Bergman, Friedenberg, and Sayegh, 1961). Ultrasonography, computed tomography, and magnetic resonance imaging frequently identify soft-tissue abnormalities of the renal pelvis but may fail to identify ureteral filling defects directly, although they may show hydronephrosis (Figure 20-6). All 3 imaging techniques differentiate blood clot and tumor from nonopaque calculi. In addition, computed tomography and magnetic resonance imaging allow simultaneous examination of abdominal and retroperitoneal structures for signs of regional (lymph node) or more distant metastases.
The use of rigid and flexible ureteropyeloscopes has allowed direct visualization of upper urinary tract abnormalities. These instruments are passed transurethrally through the ureteral orifice; in addition, they (and the similarly constructed but larger nephroscopes), can be passed percutaneously into renal calyces and the pelvis directly. The latter instrument carries with it the theoretic possibility of tumor spillage along the percutaneous tract. Indications for ureteroscopy include evaluation of filling defects within the upper urinary tract and after positive results on cytologic study or after noting unilateral gross hematuria in the absence of a filling defect. Ureteroscopy is also performed as a surveillance procedure in patients who have undergone conservative surgery for removal of a ureteral or renal pelvic tumor. Visualization, biopsy, and, on occasion, complete tumor resection, fulguration, or laser vaporization of the tumor are possible endoscopically. Detection of renal pelvic and ureteral tumors with these methods seems to be superior to that from conventional methods (Blute et al, 1989).
Treatment
Treatment of renal pelvic and ureteral tumors should be based primarily on grade, stage, position, and multiplicity. Renal function and anatomy should be assessed. The standard therapy for both tumor types has been nephroureterectomy owing to the possibility of multifocal disease within the ipsilateral collecting system. This procedure may be performed using either an open or laparoscopic approach (Landman et al, 2002; Jarrett et al, 2001). When the operation is performed for proximal ureteral or renal pelvic cancers, the entire distal ureter with a small cuff of bladder needs to be removed to avoid recurrence within this segment (Strong et al, 1976; Reitelman et al, 1987). Tumors of the distal ureter may be treated with distal ureterectomy and ureteral reimplantation into the bladder if no proximal defects suggestive of cancer have been noted (Babaian and Johnson, 1980).
Indications for more conservative surgery, including open or endoscopic excision, are not well defined. Absolute indications for renal-sparing procedures include tumor within the collecting system of a single kidney and bilateral urothelial tumors of the upper urinary tract or in patients with 2 kidneys but marginal renal function. In patients with 2 functioning kidneys, endoscopic excision alone should be considered only for low-grade and noninvasive tumors. One must realize that endoscopic examination may fail to detect the degree of infiltration adequately and therefore may understage some tumors. Limited experience with endoscopic resection, fulguration, or vaporization suggests that the procedure is safe in properly selected patients (Blute et al, 1989). However, recurrences have been noted in 15-80% of patients treated with open or endoscopic excision (Maier et al, 1990; Blute et al, 1989; Orihuela and Smith, 1988; Keeley et al, 1997; Stoller et al, 1997). Recurrence may be avoided by treating with instillation of immunotherapeutic or chemotherapeutic agents such as BCG or mitomycin C (Orihuela and Smith, 1988; Keeley and Bagley, 1997; Studer et al, 1989). These agents can be delivered to the upper urinary tract through single or double-J ureteral catheters (Patel and Fuchs, 1998). If patients are treated conservatively, it has been suggested that routine follow-up should include routine endoscopic surveillance because imaging alone may be inadequate for detecting recurrence (Chen et al, 2000).
Radiotherapy plays a limited role in upper urinary tract cancers. Although controversial, postoperative irradiation is believed by some investigators to decrease recurrence rates and improve survival in patients with deeply infiltrating cancers (Brookland and Richter, 1985; Batata et al, 1975). Patients with metastatic, transitional cell cancers of the upper urinary tract should receive cisplatin-based chemotherapeutic regimens as described for patients with metastatic bladder cancers.
Future Directions
Urothelial cancers represent a spectrum of disease defined by various recurrence and progression rates. A greater understanding of tumor induction and progression may allow the clinician to select treatments more wisely. Further development of biologic markers such as tumor proliferation or antigen expression may permit a better estimate of the biologic potential of individual tumors. More refined imaging techniques, perhaps with monoclonal antibodies, would allow clinicians to identify more advanced disease earlier and thereby select treatment strategies better. An assessment of the true benefit, if any, of either neoadjuvant or adjuvant chemotherapy awaits completion of large clinical trials. New agents for the management of most patients with metastatic disease who do not respond to conventional chemotherapy need to be developed. Mechanisms of drug resistance and the means to circumvent them need to be investigated.