Health Centers > Diabetes Center > Lactic Acidosis
Lactic Acidosis
Introduction
- Severe acidosis with hyperventilation.
- Blood pH below 7.30.
- Serum bicarbonate < 15 mEq/L.
- Anion gap > 15 mEq/L.
- Absent serum ketones.
- Serum lactate > 5 mmol/L.
General Considerations
Diabetic Coma
Diabetic Ketoacidosis
Hyperglycemic Hyperosmolar state
Lactic Acidosis
The Hypoglycemic StatesIntroduction
Hypoglycemia due to Pancreatic B cell tumors
Persistent Islet Hyperplasia(NonInsulinoma Pancreatogenous Hypoglycemia Syndrome)
Hypoglycemia Due to Extrapancreatic Tumors
Postprandial Hypoglycemia (Reactive Hypoglycemia)
Alcohol-Related Hypoglycemia
Factitious Hypoglycemia
Immunopathologic Hypoglycemia
Drug-Induced Hypoglycemia
Lactic acidosis is characterized by accumulation of excess lactic acid in the blood. Normally, the principal sources of this acid are the erythrocytes (which lack enzymes for aerobic oxidation), skeletal muscle, skin, and brain. Conversion of lactic acid to glucose and its oxidation principally by the liver but also by the kidneys represent the chief pathways for its removal. Overproduction of lactic acid (tissue hypoxia), deficient removal (hepatic failure), or both (circulatory collapse) can cause accumulation.
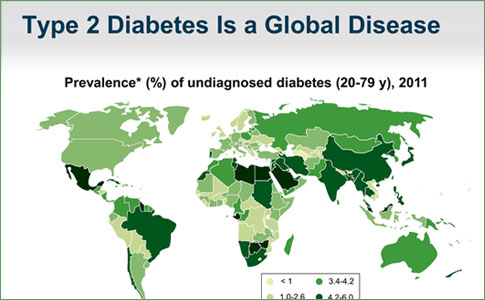
Lactic acidosis is not uncommon in any severely ill patient suffering from cardiac decompensation, respiratory or hepatic failure, septicemia, or infarction of bowel or extremities. With the discontinuance of phenformin therapy in the United States, lactic acidosis in patients with diabetes mellitus has become uncommon but occasionally occurs in metformin-treated patients and it still must be considered in the acidotic diabetic, especially if the patient is seriously ill.
Clinical Findings
A. SYMPTOMS AND SIGNS
The main clinical feature of lactic acidosis is marked hyperventilation. When lactic acidosis is secondary to tissue hypoxia or vascular collapse, the clinical presentation is variable, being that of the prevailing catastrophic illness. However, in the idiopathic, or spontaneous, variety, the onset is rapid (usually over a few hours), blood pressure is normal, peripheral circulation is good, and there is no cyanosis.
B. LABORATORY FINDINGS
Plasma bicarbonate and blood pH are quite low, indicating the presence of severe metabolic acidosis. Ketones are usually absent from plasma and urine or at least not prominent. The first clue may be a high anion gap (serum sodium minus the sum of chloride and bicarbonate anions [in mEq/L] should be no greater than 15). A higher value indicates the existence of an abnormal compartment of anions. If this cannot be clinically explained by an excess of keto acids (diabetes), inorganic acids (uremia), or anions from drug overdosage (salicylates, methyl alcohol, ethylene glycol), then lactic acidosis is probably the correct diagnosis.
In the absence of azotemia, hyperphosphatemia may be a clue to the presence of lactic acidosis for reasons that are not clear. The diagnosis is confirmed by demonstrating, in a sample of blood that is promptly chilled and separated, a plasma lactic acid concentration of 5 mmol/L or higher (values as high as 30 mmol/L have been reported). Normal plasma values average 1 mmol/L, with a normal lactate/pyruvate ratio of 10:1. This ratio is greatly exceeded in lactic acidosis.1
The Hypoglycemic States
Spontaneous hypoglycemia in adults is of two principal types: fasting and postprandial. Symptoms begin ...
1In collecting samples, it is essential to rapidly chill and separate the blood in order to remove red cells, whose continued glycolysis at room temperature is a common source of error in reports of high plasma lactate. Frozen plasma remains stable for subsequent assay.
Treatment
Aggressive treatment of the precipitating cause of lactic acidosis is the main component of therapy, such as ensuring adequate oxygenation and vascular perfusion of tissues. Empiric antibiotic coverage for sepsis should be given after culture samples are obtained in any patient in whom the cause of the lactic acidosis is not apparent.
Alkalinization with intravenous sodium bicarbonate to keep the pH above 7.2 has been recommended by some in the emergency treatment of lactic acidosis; as much as 2000 mEq in 24 hours has been used. However, there is no evidence that the mortality rate is favorably affected by administering bicarbonate, and its use remains controversial. Hemodialysis may be useful in cases where large sodium loads are poorly tolerated.
Prognosis
The mortality rate of spontaneous lactic acidosis is high. The prognosis in most cases is that of the primary disorder that produced the lactic acidosis.
Bibliography
Forsythe SM et al: Sodium bicarbonate for the treatment of lactic acidosis. Chest 2000;117:260. [PMID: 10631227]
Salpeter S et al: Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database Syst Rev 2003:CD002967. [PMID: 12804446]