Health Centers > Diabetes Center > Oral Diseases and Diabetes
Oral Diseases and Diabetes
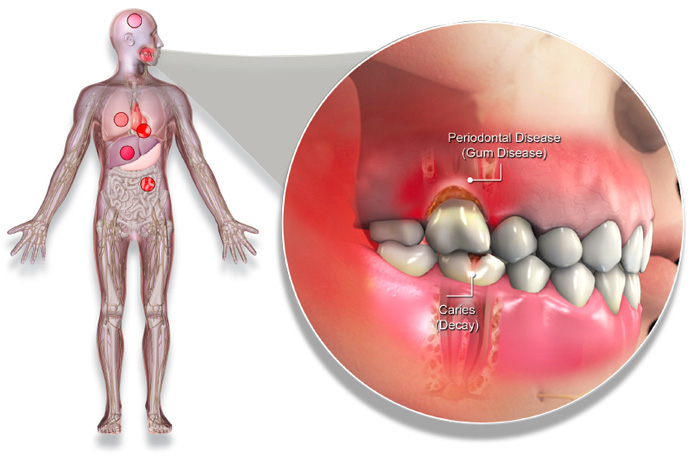
Oral conditions that are seen in individuals with diabetes may include burning mouth, altered wound healing, and an increased incidence of infection. Enlargement of the parotid glands and xerostomia can occur; both are conditions that may be related to the metabolic control of the diabetic state. Medications that diabetic patients often take for related or unrelated systemic conditions may have significant xero-stomic effects. Thus, the xerostomia seen in individuals with diabetes may result more from medications than from the diabetic condition itself.
Diabetes Mellitus and Oral Diseases
Diabetes Introduction
Diabetes Epidemiology and classification
Diabetes Pathophysiology
Clinical Presentation, Laboratory findings, and Diagnosis
Diabetes Complications
Diabetes Management
L Introduction
L Oral Agents
L Insulin
Oral Diseases and Diabetes
Periodontal Health and Diabetes
Dental Management of the Diabetic Patient
Conclusion
References
Neuropathy of the autonomic system can also cause changes in salivary secretion since salivary flow is controlled by the sympathetic and parasympathetic pathways. Dry mucosal surfaces are easily irritated and are associated with "burning mouth" syndrome; they also provide a favorable environment for the growth of fungal organisms. Some studies have shown an increased incidence of oral candidiasis in patients with diabetes whereas other studies have not.
Gum disease is one of the lesser-known complications that can affect patients with diabetes. It is estimated that 1 in 3 diabetics suffer from periodontitis at some stage of their disease
The effect of diabetes on the dental caries rate is unclear. Some studies have demonstrated increased caries in people with diabetes, which has been associated with xerostomia or increased gingival crevicular fluid glucose levels. Other studies have shown similar or decreased caries rates in people with diabetes. Since most diabetic individuals limit their intake of fermentable carbohydrates, the less cariogenic diet may limit caries incidence. In recent studies of type 2 diabetic patients and nondiabetic control subjects, no differences were seen in salivary flow rates, organic constituents of saliva, salivary counts of acidogenic bacteria, salivary counts of fungal organisms, or coronal and root caries rates. These findings suggest that diabetic individuals as a group are similar to nondiabetic people in regard to these oral conditions.
Effects of Periodontal Infection on Glycemic Control
Not only does diabetes affect the periodontium, but evidence also suggests that periodontal infection may adversely affect glycemic control of diabetes. Diabetic subjects with severe periodontal disease often have a worsening of glycemic control over time, compared to diabetic subjects without periodontitis. Periodontal infection increased the risk of poor glycemic control by sixfold in one study. Periodontitis is also associated with an increased risk for other diabetic complications, such as nephropathy and macrovascular disease. In one study, 82% of diabetic patients with severe periodontitis had at least one major cardiovascular, cerebrovascular, or peripheral vascular event during the 1- to 11-year study period, compared to only 21% of diabetic subjects with little or no periodontal disease.
The Hypoglycemic States
Spontaneous hypoglycemia in adults is of two principal types: fasting and postprandial. Symptoms begin ...
People with diabetes face a higher risk of:
Dry mouth - Uncontrolled diabetes can decrease saliva flow, resulting in dry mouth. Dry mouth can further lead to soreness, ulcers, infections, and tooth decay.
Gum inflammation (gingivitis) and periodontitis - Besides weakening white blood cells, another complication of diabetes is that it causes blood vessels to thicken. This slows the flow of nutrients to and waste products from body tissues, including the mouth. When this combination of events, the body loses its ability to fight infections. Since periodontal disease is a bacterial infection, people with uncontrolled diabetes might experience more frequent and more severe gum disease.
Poor healing of oral tissues - People with uncontrolled diabetes do not heal quickly after oral surgery or other dental procedures because blood flow to the treatment site can be damaged.
Thrush - People with diabetes who frequently take antibiotics to fight various infections are especially prone to developing a fungal infection of the mouth and tongue. The fungus thrives on the high glucose levels in the saliva of people with uncontrolled diabetes. Wearing dentures (especially when they are worn constantly) can also lead to fungal infections.
Burning mouth and/or tongue - This condition is caused by the presence of thrush.
People with diabetes who smoke are at an even higher risk - up to 20 times more likely than non-smokers to develop thrush and periodontal disease. Smoking also seems to impair blood flow to the gums, which might affect wound healing in this tissue area.
Diabetic Control. Like other complications of diabetes, gum disease is linked to diabetic control. People with poor blood sugar control get gum disease more often and more severely, and they lose more teeth than do persons with good control. In fact, people whose diabetes is well controlled have no more periodontal disease than persons without diabetes. Children with IDDM (insulin-dependent diabetes mellitus) are also at risk for gum problems. Good diabetic control is the best protection against periodontal disease.
Studies show that controlling blood sugar levels lowers the risk of some complications of diabetes, such as eye and heart disease and nerve damage. Scientists believe many complications, including gum disease, can be prevented with good diabetic control.
Blood Vessel Changes. Thickening of blood vessels is a complication of diabetes that may increase risk for gum disease. Blood vessels deliver oxygen and nourishment to body tissues, including the mouth, and carry away the tissues' waste products. Diabetes causes blood vessels to thicken, which slows the flow of nutrients and the removal of harmful wastes. This can weaken the resistance of gum and bone tissue to infection.
Bacteria. Many kinds of bacteria (germs) thrive on sugars, including glucose - the sugar linked to diabetes. When diabetes is poorly controlled, high glucose levels in mouth fluids may help germs grow and set the stage for gum disease.
Smoking. The harmful effects of smoking, particularly heart disease and cancer, are well known. Studies show that smoking also increases the chances of developing gum disease. In fact, smokers are five times more likely than nonsmokers to have gum disease. For smokers with diabetes, the risk is even greater. If you are a smoker with diabetes, age 45 or older, you are 20 times more likely than a person without these risk factors to get severe gum disease.
In diabetic patients with periodontitis, periodontal treatment may have beneficial effects on glycemic control. Several well-controlled studies of diabetic subjects with severe periodontal disease have shown improvements in glycemic control following a combination of mechanical debridement (scaling and root planing) and systemic doxycycline antibiotic therapy. Other studies in which patients received only mechanical therapy or in which the subject population already had good glycemic control prior to periodontal treatment showed no significant effect on glycemic control. The mechanisms by which adjunctive systemic antibiotics, when combined with subgingival mechanical debridement, may induce positive changes in glycemic control are presently unclear. Changes may result from more complete elimination of the subgingival pathogens in patients receiving antibiotics or from the suppression of collagenase production and AGE formation.
The oral cavity provides a continuous source of infectious agents, and its condition often reflects progression of systemic pathologies. Historically, oral infections were thought to be localized to the oral cavity except in the case of some associated syndromes and untreated odontogenic abcesses. A change in paradigm has dispelled this notion, and a whole new concept of the status of the oral cavity and its impact on systemic health and disease has evolved.
Diabetes affects > 18 million individuals in the United States and > 171 million individuals worldwide and has reached epidemic status. The disease is characterized by an increased susceptibility to infection, poor wound healing, and increased morbidity and mortality associated with disease progression. Diabetes is also recognized as an important risk factor for more severe and progressive periodontitis, infection or lesions resulting in the destruction of tissues and supporting bone that form the attachment around the tooth.
Both diseases are thought to share a common pathogenesis that involves an enhanced inflammatory response that can be observed at the local and systemic level. The inflammatory response is mainly caused by the chronic effects of hyperglycemia and specifically the formation of biologically active glycated proteins and lipids that promote inflammatory responses.