Alzheimer Disease: From Clinical Description to a Theory of Disease and Treatment
Years later, a stronger correlation was shown between cognitive impairment and reduction in synaptic density (DeKosky and Scheff 1990), but it is still not known if the age-related accumulation of amyloid plaques in the brain is a normal product of aging or a precursor of the neuritic plaques of Alzheimer disease (Knopman et al. 2003).
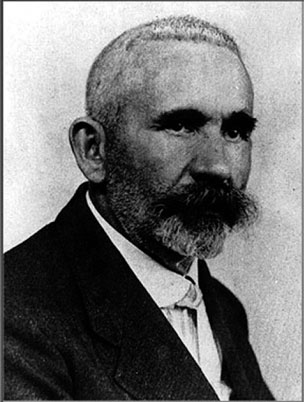 FIGURE 1-3. Emil Kraepelin, M.D., who named Alzheimer disease.Source. Department of Psychiatry, Ludwig Maximilian University Munich.
FIGURE 1-3. Emil Kraepelin, M.D., who named Alzheimer disease.Source. Department of Psychiatry, Ludwig Maximilian University Munich.
Roth and his group (Tomlinson et al. 1968, 1970) then compared the brains of older adults who displayed no objective evidence of cognitive impairment prior to death with those of persons with well-documented dementia.
Statistically significant between-group differences were found in cortical atrophy, ventricular dilatation, senile plaque formation, “Alzheimer’s neurofibrillary change,” and granulovacuolar degeneration.
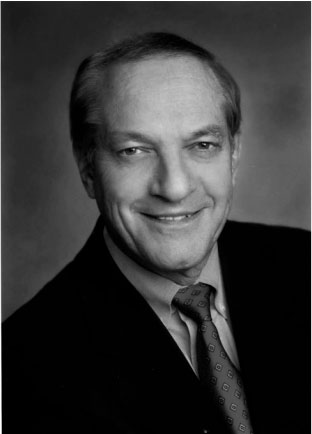 FIGURE 1-4. David A. Drachman, M.D., created a pharmacologic model of age-related cognitive change.Source. Courtesy of Dr. Drachman
FIGURE 1-4. David A. Drachman, M.D., created a pharmacologic model of age-related cognitive change.Source. Courtesy of Dr. Drachman
Because memory impairment is typically the presenting symptom of Alzheimer disease, researchers attempted to understand and treat this symptom by integrating the biology of memory with the pathophysiology of Alzheimer disease. Deutsch (1971) suggested that the cholinergic system is the biological substrate of memory. Subsequently, David Drachman (Figure 1-4) (Drachman and Leavitt 1974) showed that scopolamine blocked storage in long-term memory with relative sparing of recall and retrieval from long-term memory, a pattern similar to that of normal aging.
Searching for the relationship between neuropathology and brain function, Davies and Maloney (1976) assayed postmortem levels of enzymes associated with the neurotransmitters acetylcholine, γ -aminobutyric aid (GABA), dopamine, noradrenaline, and 5-hydroxytryptamine in 3 subjects with Alzheimer disease and 10 control subjects. Levels of choline acetyltransferase, the enzyme forming acetylcholine, and acetylcholinesterase, which hydrolyzes acetylcholine in the synapse, were dramatically reduced in the Alzheimer brains; the level of reduction coincided with the areas containing the greatest number of neurofibrillary tangles. The following year, White et al. (1977) confirmed that the presynaptic cholinergic marker choline acetyltransferase was reduced in subjects with Alzheimer disease, but also found intact postsynaptic receptor binding, suggesting that treatment with centrally acting cholinesterases might be beneficial before neuronal loss was advanced. The potential utility of this approach was underscored by the finding of massive cell loss in Alzheimer disease in basal forebrain nuclei, including the nucleus basalis of Meynert, a poorly defined group of neurons located dorsal to the optic chiasm that supplies most of the cholinergic innervation to the cerebral cortex (Whitehouse et al. 1981).
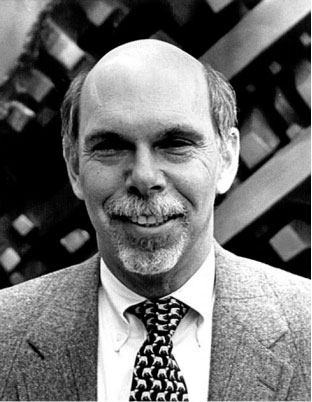 FIGURE 1-5. Kenneth L. Davis, M.D., showed memory-enhancing property of physostigmine.Source. Courtesy of Dr. Davis.
FIGURE 1-5. Kenneth L. Davis, M.D., showed memory-enhancing property of physostigmine.Source. Courtesy of Dr. Davis.
Experimentation with the anticholinesterase physostigmine by Kenneth Davis (Figure 1-5) led to the observation that it improved memory in cognitively intact individuals (Davis et al. 1978) and persons with Alzheimer disease (Davis and Mohs 1982), but the short half-life of this drug and the need for parenteral administration made it unsuitable for clinical use. At the same time, the longacting cholinesterase inhibitor tacrine was being investigated clinically, following the clinical observation that it effectively reversed anticholinergic delirium following overdose of tricyclic antidepressants (Summers et al. 1981). Following the publication of a large multicenter study by Davis et al. (1992), the U.S. Food and Drug Administration approved tacrine for the treatment of Alzheimer disease in 1993. Other cholinesterase inhibitors were later approved, and the use of tacrine gradually vanished because of the need for frequent dosing, slow titration, and hepatotoxicity. Overall, these drugs produce small, transient cognitive improvement and modest, if any, effect on disease progression, as would be expected from a symptomatic treatment.
The 1980s saw progress in elucidating the neuropathology and pathophysiology of Alzheimer disease. Glenner and Wong (1984a) sequenced from blood vessel deposits of patients with Alzheimer disease the substance that had been recognized in the core of neuritic plaques as amyloid protein (Terry et al. 1964). Based on work published the previous year showing the presence of Alzheimer disease pathology to be ubiquitous in persons with Down syndrome who had reached age 40 years, Glenner and Wong (1984b) showed that the amyloid in Down syndrome was identical to that found in patients with Alzheimer disease. Korenberg et al. (1989) later showed that the portion of chromosome that is reduplicated in trisomy 21 Down syndrome contains the amyloid precursor protein, suggesting that the cause of Alzheimer disease in these persons is overloading of the proteolytic pathway of normal amyloid precursor protein. The subsequent work in molecular genetics began with the localization of a gene for familial Alzheimer disease to chromosome 21 (St. George-Hyslop et al. 1987).
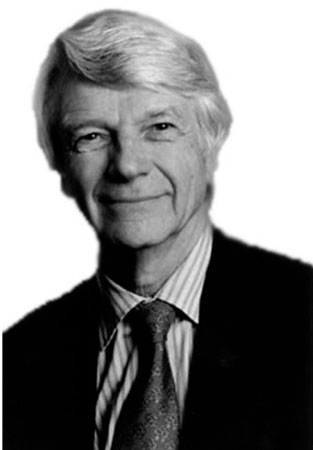 FIGURE 1-6. Robert N. Butler, M.D., first head of the National Institute on Aging.
FIGURE 1-6. Robert N. Butler, M.D., first head of the National Institute on Aging.
Source. Courtesy of the International Longevity Center.