Vascular Diseases
The vascular system is the network of blood vessels that circulate blood to and from the heart and lungs. Vascular diseases are very common, especially as people age. Many people have these diseases and don’t know it, because they rarely cause symptoms in the early stages. People with risk factors or any signs or symptoms of vascular disease, should be evaluated by a physician. Untreated vascular disease can lead to serious health problems, such as tissue death and gangrene requiring amputation or other surgery; chronic disability and pain; and weakened blood vessels that may rupture without warning. Deadly complications can result, including stroke (a clogged or narrowed blood vessel cuts the supply of blood to the brain), and Pulmonary embolism (a blood clot breaks loose and travels to the heart and lungs).
Vascular Diseases Overview
- Vascular Diseases Overview
- The Blood Vessels
- Preventing Vascular Disease
- Arterial Disease and Venous Disease
- Arterial Disease
- Blood Clots and Deep Vein Thrombosis (DVT)
- Deep Vein Thrombosis
- Risk Factors for Venous Disease
- Vascular Diseases Diagnosis
- Symptoms of Varicose Veins
- Diagnosing Venous Disease and Pulmonary Embolism
- Diagnosing Pulmonary Embolism
- Vascular Diseases Treatments
- Catheter-Directed Thrombolysis
- Treatments For Varicose Veins
- Treatments for Phlebitis
- Treatments for Venous Stasis Disease
- Treatments for Pulmonary Embolism
The Circulatory System
The blood vessels that comprise the vascular system are part of the circulatory, or cardiovascular, system. The heart is the major organ of this system. With each beat, it pumps blood into the vessels and through the body, bringing oxygen and other nutrients necessary to the life to the cells. As the blood circulates, it also removes waste products, toxins and other harmful substances. The circulatory system works with many other systems. It plays an especially important role in:
- The Respiratory System. Blood circulates through the lungs where it exchanges carbon dioxide and oxygen.
- The Digestive System. Blood circulates through the intestines where it absorbs nutrients from food that was eaten and digested.
- The Excretory System. Blood circulates through the kidneys which filter out wastes that are removed from the body in the urine.
- Temperature Control. As the blood flows, heat moves back and forth between the blood and the cells. This constant exchange of heat keeps all the body parts at the same temperature. This explains why people with circulatory problems often have cold feet or hands, or spots where the skin is warm to the touch.
There are three types of vessels that aid in the transport of blood, and in keeping it in constant circulation from the heart to the body, and back to the heart:
- Arteries
- Veins
- Capillaries
The blood vessels are more than simple tubes through which blood flows. Each has its own characteristics, depending on the role it plays in the circulatory system.
Arteries are strong, flexible blood vessels that must expand to accept the blood pumped into them with each beat of the heart, and contract to squeeze blood into the veins when the heart relaxes.
Veins The veins that return blood to the heart are less “active” and elastic than the arteries. Veins have valves that open to let blood through, and close to prevent blood from pooling in the legs and elsewhere due to the pull of gravity. There are three types of veins:
Capillaries, which look more like webs than vessels or tubes, lie in tangled “beds” in the tissues of the body. They are so tiny that blood cells must pass through them in single file. The exchange between the blood and the cells of the body takes place in the capillary beds. Here, blood takes oxygen from the cells and gives up carbon dioxide. Special capillaries in the kidneys, liver and elsewhere take waste products that are excreted from the body. As the capillaries spread out of their beds, they thicken and merge into small vessels called “venules” that, in turn, lead to larger veins that return blood to the heart.
The best way to prevent vascular disease is to live a “heart healthy” lifestyle – don’t smoke; eat nutritious, low fat foods; exercise; control risk factors and maintain a healthy weight.
Types of Vascular (Blood Vessel) Disease
Most vascular diseases are caused by conditions that clog or weaken blood vessels, or damage valves that control the flow of blood in and out of the veins. Most vascular disease is caused by arteriosclerosis, often called “hardening of the arteries” (although veins also can be affected).
In this condition, a sticky substance called “plaque” builds up inside the blood vessels. Over time, the blood vessels may weaken or become so clogged that the blood supply to affected parts of the body is reduced or blocked. The flow of blood also may be affected when a blood clot (thrombus) gets stuck in a blood vessel.
Arterial Disease and Venous Disease
It is called “arterial disease” when arteriosclerosis, blood clots and other vascular conditions occur in the arteries. Problems that occur in the veins are called “venous disease.” Some vascular conditions occur only in arteries, others are unique to the veins. Some can affect either type of vessel, such as aneurysms and Arteriovenous malformations (AVM) (abnormalities in the brain or elsewhere in which the blood vessels are tangled and distended). Aneurysm and AVMS are called “silent killers” because they often produce no symptoms until they rupture.

Aneurysms are weakened areas in the blood vessels that bulge like balloons when blood flows through them. Once they grow to a certain size, there is a risk of rupture and life-threatening bleeding.
Common diseases affecting the arteries include:
- Peripheral vascular disease (PVD) (sometimes called Peripheral arterial disease, or PAD) is a condition where the arteries that carry blood to the legs (and, less frequently, the arms) become narrow or clogged.
- Carotid artery disease is a condition in which the arteries in the neck that supply blood to the brain become clogged and may cause a stroke.
- Abdominal aortic aneurysm (AAA), or Triple A, is an area in the main artery of the heart (the aorta) that is weakened and bulges like a balloon. If it grows large enough, the aneurysm can rupture and cause life-threatening bleeding. Males over the age of 60 who smoke or have ever smoked and people with a history of AAA in their family are at highest risk for this disease.
Venous Disease
Common conditions affecting the veins include:
- Blood Clots, Deep Vein Thrombosis (DVT)
- Venous Stasis Disease
- Phlebitis
- Varicose Veins (also called “varicoceles”)
These conditions usually occur in the veins of the legs.
Blood Clots and Deep Vein Thrombosis (DVT)
The tendency of blood cells to “stick together” and form clots depends on a combination of two factors:
1. Sluggish Blood Flow. Sitting still or lying down for a long time, such as on an airplane ride, can slow down the flow of blood. Prolonged bed rest after surgery or injury is especially likely to contribute to blood clots.
2. Clotting Factors. Clotting factors – substances in the blood that regulate the formation of clots – may increase after an operation or injury, or during pregnancy. Talking birth control pills may increase a woman’s risk of forming blood clots. Severe infection, an increase in red cells, certain types of cancer and an injury to the vein itself are other factors that can contribute to the formation of blood clots.
The deep veins that lie near the center of the leg do most of the work of the venous system. Nearly all – 85 percent – of the circulating blood is returned to the heart through these veins. DVT – the formation of a clot (or thrombus) in any one of these veins – can be a very serious problem. Typically, the clot comes on suddenly and without warning. If not treated, DVT can block the blood supply to the legs and cause tissue death or gangrene that requires the removal (amputation) of all or part of the leg. DVT also can lead to valve damage in the vein and a chronic condition, called venous stasis disease, that is difficult to treat.
DVT may be related to prolonged periods of bed rest or inactivity, injury to the vein, surgery or pregnancy.
In addition to restricting the flow of blood, there is risk that the clot may break off, travel through the heart and get trapped in the lung (Pulmonary embolism) – a potentially fatal complication.
Risk Factors for Venous Disease
Factors that increase the chances of venous disease include:
- A family history.
- Increasing age that results in a loss of elasticity in the veins and their valves.
- Pregnancy.
- Illness or injury.
- Prolonged periods of inactivity – sitting, standing or bed rest.
- Hypertension, diabetes, High cholesterol or other conditions that affect the health of the cardiovascular system.
- Smoking.
- Obesity.
==============
Vascular Diseases Diagnosis
What are the Symptoms of Vein Disease?
There may be no symptoms of venous disease caused by blood clots until the clot grows large enough to block the flow of blood through the vein. Symptoms may then come on suddenly:
- pain
- sudden swelling in the affected limb
- enlargement of the superficial veins
- reddish-blue discoloration
- skin that is warm to the touch
Swelling and discoloration of the leg is a sign of Deep Vein Thrombosis
Swelling and discoloration of the leg is a sign of Deep Vein Thrombosis
What are the symptoms of Pulmonary Embolism?
- a sudden feeling of apprehension
- shortness of breath
- sharp chest pain
- rapid pulse
- sweating
- cough with bloody sputum
- fainting
Varicose veins , also called “varicoceles,” result when the valves that control the flow of blood in and out of veins fail to work properly and the pull of gravity causes blood to pool in the legs or elsewhere. Varicoceles in the scrotum may cause infertility in men. Varicoceles in the veins of the ovaries may cause chronic pelvic pain in some women.
When valves fail in the legs, the superficial veins become enlarged and twisted, where they appear as twisted, dark blue vessels just under the skin’s surface. Smaller varicose veins are sometimes called spider veins. Obesity, pregnancy, constriction of the veins with garters or tight clothing, and an inherited tendency are among the contributing causes of varicose veins. Usually, there are no symptoms. Varicose veins are diagnosed by physical examination.
Most varicose veins have no symptoms other than the appearance of purplish, knotted veins on the surface of the skin. A physician should be consulted and treatment may be required if there is:
- pain or heaviness in the leg, feet and ankles,
- swelling,
- sores or ulcers on the skin, or
- severe bleeding if the vein is injured.
Phlebitis is an inflammation of a vein that can be due to bacterial infection, injury or unknown causes. Thrombophlebitis is inflammation that results from the formation of a blood clot in an arm or leg vein. It can occur in a superficial vein near the skin surface or in a deep vein. Pain and inflammation are the most common symptoms. Unfortunately, in the case of thrombophlebitis in the deep veins (see deep vein thrombosis) there may be no symptoms unless the clot travels to the lungs, resulting in a life-threatening Pulmonary embolism.
Venous stasis disease also is caused by defective values in the veins, but it is far more serious than varicose veins. If a damaged valve does not close completely, pooled blood can build up in the veins causing pain, swelling and tissue damage that may lead to painful sores or ulcers. Chronic venous stasis disease can result in devastating disfigurement, disability and a lifetime of treatments and hospital stays. Fortunately, early diagnosis and treatment can avoid these long-term effects.
Diagnosing Venous Disease and Pulmonary Embolism
Venous disease is diagnosed using one or more of the following techniques:
Duplex or Doppler Ultrasound – This non-invasive technique uses ultrasound to “see” clots or other abnormalities in the blood vessels.
Ultrasound is a technique in which a “transducer” (a hand held device about the size of a computer mouse) is moved over the skin and harmless sound waves “bounce” back signals that are computerized to create an image. The technique is painless and has no known risk. Here, a “colorized” ultrasound image highlights the blood vessels.
Ultrasound is a technique in which a “transducer” (a hand held device about the size of a computer mouse) is moved over the skin and harmless sound waves “bounce” back signals that are computerized to create an image. The technique is painless and has no known risk. Here, a “colorized” ultrasound image highlights the blood vessels.
CT Scan (Computed Tomography) is similar to an X-ray except the images are computerized to appear as a series of slides. When viewed together, the slices provide a three-dimensional image. Sometimes a special dye, or contrast agent, is injected or swallowed before the exam to highlight the images.
Venography is a type of X-ray (called angiography) in which a thin, flexible tube, or catheter, is threaded into the blood vessels. A local anesthetic is given to numb the skin where the catheter is inserted, and X-rays are used to guide the catheter. A contrast agent, or dye, is injected through the catheter to highlight the blood vessel and call attention to any abnormalities. This procedure is performed by an interventional radiologist – a specialist who diagnoses and treats many vascular diseases and other conditions without surgery.
Magnetic Resonance Angiography (MRA) is a noninvasive exam in which a magnetic resonance (MR) scanner uses harmless but powerful magnetic fields and radio waves to create detailed images of the blood vessels.
A V/Q scan (sometimes called a V/P or ventilation/perfusion scan) is a nuclear medicine test in which short-acting radioactive particles are injected through a vein or breathed into the lungs. If there are areas of the lung that do not “take up” the particles, it is an indication that there may be a blood clot. Computed tomography (CT), chest X-rays or venography also may be used to diagnose blood clots in the lung.
Vascular Diseases Treatments
Treatments for Deep Vein Thrombosis
The traditional treatments for DVT are:
- bed rest
- elevation of the affected limb
- pressure stockings, and
- drugs to prevent blood from clotting. These drugs, called anticoagulants, keep the clot from growing larger and may prevent clots from breaking off to travel to the lungs – called Pulmonary embolism. But they cannot dissolve clots that already have formed. These must be dissolved over time by the body’s own system for breaking down clots, or by a new technique called:
Catheter-Directed Thrombolysis
This procedure dissolves blood clots in the veins without surgery. “Clot busting” drugs (thrombolytic agents) are injected directly into the site of the clot (the deep vein thrombus).
Catheter-directed thrombolysis usually is performed in a hospital radiology suite by an interventional radiologist. The physician inserts the catheter into a vein in the leg and threads it to the site of the clot. With his special training as a radiologist, the doctor is able to expertly guide and watch the progress of the procedure on an X-ray video monitor. When the catheter tip is in the clot, the clot-dissolving drug is sent (infused) through the catheter tube. In most cases, it takes a few days for the clot to completely dissolve. The interventional radiologist can “see” and monitor the treatment using special X-rays, called venograms, and ultrasound scans. With X-ray and ultrasound pictures, the physician also can see if – after the clot dissolves – the vein wall is narrowed or damaged, which can lead to more clots in the future.
Balloon Angioplasty and Stenting. If a vein has been narrowed or damaged, it may be necessary for the interventional radiologist or other physician to perform balloon angioplasty, a procedure in which a catheter is placed in the vein under X-ray guidance to the site of the narrowing, and a balloon is inflated to press open the narrowed blood vessel. In many cases, a small mesh cylinder called a stent may be inserted through the catheter and left behind in the vein to keep it open.
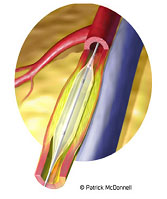
Balloon Angioplasty: A catheter is directed into the blood vessel and a balloon is inflated to press open the narrowed wall.
Behavioral changes can help prevent the formation of varicose veins.
- Cross the legs at the ankles instead of the knees when sitting
- Avoid high heels, which limit the use of the calf muscles.
- Avoid restrictive clothing which limit blood flow in the groin or calf.
- Avoid prolonged sitting or standing.
- Take breaks to elevate the legs or walk around to help move the blood along and prevent valve failure.
Existing varicose veins won’t get better without treatment
Treatment may consist of:
- Rest.
- Elevation of the leg.
- External support such as elastic wraps or support hose. Elastic stockings are preferred over elastic bandages.
- Laser treatment. A new laser treatment is being provided by interventional radiologists as an alternative to surgical treatments. The EndoVenous Laser Treatment uses a laser fiber to heat and seal the main vein that is causing the varicosity.
- RF Energy. Radiofrequency (RF) energy is another new technique provided by interventional radiologists as an alternative to surgery. RF energy heats the problem vein from the inside, shrinking it. Nearby veins take over.
- Sclerotherapy. In this treatment, a thin tube called a catheter is directed to the vein and a substance is injected that causes the veins to scar and close – rerouting the blood to healthier veins. The affected vein forms a knot of scar tissue that is absorbed by the body over time.
- Phlebectomy. In this procedure, varicose veins are removed through a series of small holes in the skin under local anesthesia.
- Vein stripping involves removal of a long vein through small incisions in the skin.
- Endoscopic repair. This procedure is performed in advanced cases of vascular disease involving sores or ulcers on the legs. Surgeons insert an endoscopic camera into the varicose vein via small incisions to visualize and treat the defects.
Thrombophlebitis in the superficial veins is generally treated at home with periods of rest with the leg elevated, pain relievers such as aspirin and, if needed, antibiotics. Warm compresses may ease the inflammation and elastic stockings may be prescribed.
Deep vein thrombophlebitis is treated with anticoagulants (drugs that prevent the blood from clotting) or with thrombolysis, a procedure in which clot busting drugs are infused to the site of a blood clot. This procedure usually is performed by an interventional radiologist.
Treatments for Venous Stasis Disease
Over time, untreated DVT or other conditions may damage a valve in the vein so that it does not close completely. When this occurs, blood flows back into the vein below the valve and collects in the lower leg veins. Pooling of blood in these lower leg veins may cause swelling and tissue damage and lead to painful sores or ulcers. This condition is known as venous stasis disease.
Fortunately, prompt treatment of DVT or other vein disease can prevent complications such as Pulmonary embolism and venous stasis disease.
Treatments for Pulmonary Embolism
Pulmonary Embolism is a common event, especially in hospitalized patients. It is estimated that more than 600,000 new cases of Pulmonary embolism occur in the United States each year and 200,000 people die of the disorder. Treatment options include:
- Anticoagulation. Blood thinners are prescribed to prevent the clot from growing or new clots from forming while the body dissolves the existing clot on its own.
- Vena cava filters are devices that are placed in some patients when there is a possibility of recurrent blood clots, or emboli, or in patients with chronic pulmonary disease to prevent further damage to the blood vessels of the lungs. Vena cava filters usually are placed by physician specialists called interventional radiologists who perform procedures without surgery by guiding catheters and other small instruments through the blood vessels under X-ray guidance.
- Thrombolytic therapy, is another interventional radiology technique in which clot busting drugs are fed (infused) through a catheter directly to the site of the blood clot in the lung.
- Percutaneous thrombectomy. In this procedure, a catheter is sent to the site of the clot under X-ray guidance and a device is used to break up the clot into small pieces that are easily absorbed by the body.
Revision date: July 7, 2011
Last revised: by Andrew G. Epstein, M.D.