Health Centers > Disorders of Blood Vessels and Lymphatics > Peripheral Arterial Disease
Peripheral Arterial Disease
Introduction
Peripheral arterial disease (PAD) involves the atherosclerotic occlusion of the arterial circulation to the lower extremities. The disease may be asymptomatic (identified only by a reduced blood pressure in the ankle), or it may manifest symptoms of intermittent claudication or severe chronic leg ischemia. The typical patient with PAD presents a decade later than the patient with coronary artery disease and experiences a profound limitation in exercise capacity and quality of life. In addition to affecting the limbs, PAD is a manifestation of systemic atherosclerosis affecting other major circulations involving the cerebral and coronary circulations. Thus, all patients with PAD are at an increased risk of cardiovascular morbidity and mortality. The treatment goals are directed at providing symptom relief and at reducing the risk of systemic cardiovascular morbidity and mortality.
Epidemiology
In the Framingham study, subjects were assessed for PAD using a history of claudication as a marker of the disease. Men and women had a similar incidence of intermittent claudication, which increased with age. However, symptoms underestimate the true incidence and prevalence of the disease. Using the ankle-brachial index (ABI; described later), the prevalence of PAD is quite high, affecting 12% of the adult population and 20% of individuals over the age of 70. These figures extrapolate to approximately 8 million persons affected with PAD in the United States.
The natural history of PAD has been evaluated in several studies. These studies have shown that elderly control subjects had an all-cause mortality rate of 1.6% per year. This rate was increased to 4.8% per year in patients with PAD, a 2.5-fold increased risk. Cardiovascular mortality rates are similarly affected, with 3- to 4-fold increased risk for patients with PAD. Importantly, women are at approximately the same risk as men, and even asymptomatic individuals, who are identified solely based on an abnormal ankle-brachial index (ABI), have a markedly increased risk of cardiovascular events. The mortality risk in patients with PAD is maintained after adjustment for other cardiovascular risk factors and even in patients with known coronary artery disease.
What is peripheral arterial disease of the legs?
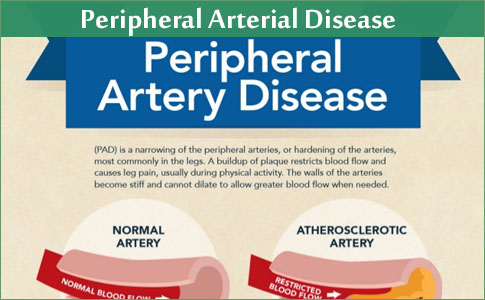
Peripheral arterial disease (PAD) is poor blood flow in the arteries. The arteries carry blood to the organs and muscles. If arteries get narrowed or blocked because of disease, the muscles and organs may not get enough blood to work properly.
PAD increases your chance of having a heart attack or stroke. People with PAD are 3 to 4 times more likely to die from a stroke or heart attack than people of the same age who do not have PAD.
What causes PAD?
The most common cause is the buildup of plaque on the inside of arteries. Plaque is made of extra cholesterol, calcium, and other material in your blood. Over time, plaque builds up along the inner walls of the arteries, including those that supply blood to your legs.
If plaque builds up in your arteries, there is less room for blood to flow. Every part of your body needs blood that is rich in oxygen. But plaque buildup prevents that blood from flowing freely and starves the muscles and other tissues in the lower body.
This process of plaque buildup usually happens at the same time throughout the body. It is called atherosclerosis or hardening of the arteries. If you have this problem in your legs, you most likely will have it in the arteries that supply blood to your heart and brain. These arteries are called coronary arteries and carotid arteries.
Plaque builds up bit by bit over a lifetime, but symptoms often do not start until after age 65. High cholesterol, high blood pressure, and smoking make you more likely to get atherosclerosis and peripheral arterial disease.
Women & Vascular Disease
Heart disease is the #1 killer of women in the United States. Like heart disease, peripheral arterial disease is under-recognized in women. Through early detection, the progression of vascular disease can be halted, saving women from future stroke, heart attack, and early death if PAD is detected early.
What is the outlook (prognosis) for peripheral arterial disease?
Studies that have followed-up people with PAD have shown that:
- Symptoms remain stable or improve in about 15 out of 20 cases.
- Symptoms gradually become worse in about 4 out of 20 cases.
- Symptoms become severe in about 1 out of 20 cases.
So, in most cases, the outlook for the legs is quite good. However, if you have PAD it means that you have an increased risk of developing atheroma in other arteries. Therefore, you have a higher than average risk of developing heart disease (such as angina or a heart attack), or of having a stroke. The main concern for most people with PAD is not that they might need an amputation - but the increased risk of having a heart attack or stroke.
The chance of developing severe PAD (and heart disease, or a stroke) is much reduced by the self help measures and treatments described below.
References
1. Kannel WB, McGee DL. Update on some epidemiologic features of intermittent claudication: the Framingham Study. J Am Geriatr Soc. 1985;33:13-18.
2. Hiatt WR, Hoag S, Hamman RF. Effect of diagnostic criteria on the prevalence of peripheral arterial disease. The San Luis Valley diabetes study. Circulation. 1995;91:1472- 1479.
3. Criqui MH, Langer RD, Fronek A, et al. Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med. 1992;326:381-386.
4. Vogt MT, Cauley JA, Newman AB, Kuller LH, Hulley SB. Decreased ankle/arm blood pressure index and mortality in elderly women. JAMA. 1993;270:465-469.
5. Newman AB, Tyrrell KS, Kuller LH. Mortality over four years in SHEP participants with a low ankle-arm index. J Am Geriatr Soc. 1997;45:1472-1478.
6. Leng GC, Fowkes FG, Lee AJ, et al. Use of ankle brachial pressure index to predict cardiovascular events and death: a cohort study. Br Med J. 1996;313:1440-1444.
7. Leng GC, Lee AJ, Fowkes FG, et al. Incidence, natural history and cardiovascular events in symptomatic and asymptomatic peripheral arterial disease in the general population. Int J Epidemiol. 1996;25:1172-1181.
8. Eagle KA, Rihal CS, Foster ED, Mickel MC, Gersh BJ. Long-term survival in patients with coronary artery disease: importance of peripheral vascular disease. The Coronary Artery Surgery Study (CASS) Investigators. J Am Coll Cardiol. 1994;23:1091-1095.
9. Vogt MT, Cauley JA, Kuller LH, Hulley SB. Prevalence and correlates of lower extremity arterial disease in elderly women. Am J Epidemiol. 1993;137:559-568.
10. Beach KW, Strandness DE. Arteriosclerosis obliterans and associated risk factors in insulin-dependent and non-insulin-dependent diabetes. Diabetes. 1980;29:882-888.
11. Murabito JM, D'Agostino RB, Silbershatz H, Wilson WF. Intermittent claudication. A risk profile from The Framingham Heart Study. Circulation. 1997;96:44-49.
12. Quick CRG, Cotton LT. The measured effect of stopping smoking on intermittent claudication. Br J Surg. 1982;69(suppl):S24-S26.
13. Stewart CP. The influence of smoking on the level of lower limb amputation. Prosthet Orthot Int. 1987;11:113-116.
14. Malinow MR, Kang SS, Taylor LM, et al. Prevalence of hyperhomocyst(e)inemia in patients with peripheral arterial occlusive disease. Circulation. 1989;79:1180-1188.
15. Hoogeveen EK, Kostense PJ, Beks PJ, et al. Hyperhomocysteinemia is associated with an increased risk of cardiovascular disease, especially in non-insulin-dependent diabetes mellitus: a population-based study. Arterioscler Thromb Vasc Biol. 1998;18:133-138.
16. Welch GN, Loscalzo J. Homocysteine and atherothrombosis. N Engl J Med. 1998;338:1042-1050.
17. Lee AJ, Lowe GDO, Woodward M, Tunstall-Pedoe H. Fibrinogen in relation to personal history of prevalent hypertension, diabetes, stroke, intermittent claudication, coronary heart disease, and family history: the Scottish Heart Health Study. Br Heart J. 1993;69:338-342.
18. Donaldson MC, Weinberg DS, Belkin M, Whittemore AD, Mannick JA. Screening for hypercoagulable states in vascular surgical practice: a preliminary study. J Vasc Surg. 1990;11:825-831.
19. Catalano M, Russo U, Libretti A. Plasma beta- thromboglobulin levels and claudication degrees in patients with peripheral vascular disease. Angiology. 1986;37:339- 342.
20. England JD, Regensteiner JG, Ringel SP, Carry MR, Hiatt WR. Muscle denervation in peripheral arterial disease. Neurology. 1992;42:994-999.
21. Regensteiner JG, Wolfel EE, Brass EP, et al. Chronic changes in skeletal muscle histology and function in peripheral arterial disease. Circulation. 1993;87:413-421.
22. Hiatt WR, Wolfel EE, Regensteiner JG, Brass EP. Skeletal muscle carnitine metabolism in patients with unilateral peripheral arterial disease. J Appl Physiol. 1992;73:346-353.
23. Bhat HK, Hiatt WR, Hoppel CL, Brass EP. Skeletal muscle mitochondrial DNA injury in patients with unilateral peripheral arterial disease. Circulation. 1999;99:807-812.
24. Brass EP, Hiatt WR. Acquired skeletal muscle metabolic myopathy in atherosclerotic peripheral arterial disease. Vasc Med. 2000;5:55-59.
25. Brass EP, Hiatt WR, Gardner AW, Hoppel CL. Decreased NADH dehydrogenase and ubiquinol-cytochrome c oxidoreductase in peripheral arterial disease. Am J Physiol. 2001;280:H603-H609.
26. Bauer TA, Regensteiner JG, Brass EP, Hiatt WR. Oxygen uptake kinetics during exercise are slowed in patients with peripheral arterial disease. J Appl Physiol. 1999;87:809-816.
27. Hirsch AT, Criqui MH, Treat-Jacobson D, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286(11):1317-1324.
28. Carter SA. Clinical measurement of systolic pressures in limbs with arterial occlusive disease. JAMA. 1969;207:1869- 1874.
29. Hiatt WR, Hirsch AT, Regensteiner JG, Brass EP. Clinical trials for claudication. Assessment of exercise performance, functional status, and clinical end points. Vascular Clinical Trialists. Circulation. 1995;92:614-621.
30. Regensteiner JG, Steiner JF, Hiatt WR. Exercise training improves functional status in patients with peripheral arterial disease. J Vasc Surg. 1996;23:104-115.
31. Jonason T, Bergstrom R. Cessation of smoking in patients with intermittent claudication. Acta Med Scand. 1987;221:253-260.
32. Jorenby DE, Leischow SJ, Nides MA, et al. A controlled trial of sustained-release bupropion, a nicotine patch, or both for smoking cessation. N Engl J Med. 1999;340:685- 691.
33. Joseph AM, Norman SM, Ferry LH, et al. The safety of transdermal nicotine as an aid to smoking cessation in patients with cardiac disease. N Engl J Med. 1996;335:1792- 1798.
34. Effect of intensive diabetes management on macrovascular events and risk factors in the Diabetes Control and Complications Trial. Am J Cardiol. 1995;75:894-903.
35. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352:837-853.
36. Estacio RO, Jeffers BW, Hiatt WR, et al. The effect of nisoldipine as compared with enalapril on cardiovascular outcomes in patients with non-insulin-dependent diabetes and hypertension. N Engl J Med. 1998;338:645-652.
37. DeFronzo RA. Pharmacologic therapy for type 2 diabetes mellitus. Ann Intern Med. 1999;131:281-303.
38. Elam MB, Hunninghake DB, Davis KB, et al. Effect of niacin on lipid and lipoprotein levels and glycemic control in patients with diabetes and peripheral arterial disease: the ADMIT study: a randomized trial. Arterial Disease Multiple Intervention Trial. JAMA. 2000;284:1263-1270.
39. Leng GC, Price JF, Jepson RG. Lipid-lowering for lower limb atherosclerosis (Cochrane Review). In; The Cochrane Library. Oxford; Update Software; 1999.
40. Summary of the second report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel II). JAMA. 1993;329:3015- 3023.
41. Ansell BJ, Watson KE, Fogelman AM. An evidence-based assessment of NCEP Adult Treatment Panel II guidelines. National Cholesterol Education Program. JAMA. 1999;282:2051-2057.
42. The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med. 1997;157:2413-2446.
43. Hiatt WR, Stoll S, Nies AS. Effect of β-adrenergic blockers on the peripheral circulation in patients with peripheral vascular disease. Circulation. 1985;72:1226-1231.
44. Radack K, Deck C. Beta-adrenergic blocker therapy does not worsen intermittent claudication in subjects with peripheral arterial disease. A meta-analysis of randomized controlled trials. Arch Intern Med. 1991;151:1769-1776.
45. Poldermans D, Boersma E, Bax JJ, et al. The effect of bisoprolol on perioperative mortality and myocardial infarction in high-risk patients undergoing vascular surgery. N Engl J Med. 1999;341:1789-1794.
46. The Heart Outcomes Prevention Evaluation Study Investigators. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000;342:145-153.
47. Jacques PF, Selhub J, Bostom AG, Wilson PW, Rosenberg IH. The effect of folic acid fortification on plasma folate and total homocysteine concentrations. N Engl J Med. 1999;340:1449-1454.
48. The Writing Group for the PEPI Trial. Effects of estrogen or estrogen/progestin regimens on heart disease risk factors in postmenopausal women. The Postmenopausal Estrogen/ Progestin Interventions (PEPI) Trial. JAMA. 1995;273:199- 208.
49. Hulley S, Grady D, Bush T, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. Heart and Estrogen/Progestin Replacement Study (HERS) Research Group. JAMA. 1998;280:605-613.
50. Antiplatelet Trialists' Collaboration. Secondary prevention of vascular disease by prolonged antiplatelet treatment. Br Med J. 1988;296:320-331.
51. Antiplatelet Trialists' Collaboration. Collaborative overview of randomised trials of antiplatelet therapy. I: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Br Med J. 1994;308:81-106.
52. Antiplatelet Trialists' Collaboration. Collaborative overview of randomised trials of antiplatelet therapy. II: Maintenance of vascular graft or arterial patency by antiplatelet therapy. Br Med J. 1994;308:159-168.
53. Bokissel JP, Peyrieux JC, Destors JM. Is it possible to reduce the risk of cardiovascular events in subjects suffering from intermittent claudication of the lower limbs? Thromb Haemostasis. 1996;62:681-685.
54. Arcan JC, Blanchard J, Boissel JP, Destors JM, Panak E. Multicenter double-blind study of ticlopidine in the treatment of intermittent claudication and the prevention of its complications. Angiology. 1988;39:802-811.
55. CAPRIE Steering Committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet. 1996;348:1329-1339.
56. Gardner AW, Poehlman ET. Exercise rehabilitation programs for the treatment of claudication pain. A meta-analysis. JAMA. 1995;274:975-980.
57. Coffman JD. Vasodilator drugs in peripheral vascular disease. N Engl J Med. 1979;300:713-717.
58. Porter JM, Cutler BS, Lee BY, et al. Pentoxifylline efficacy in the treatment of intermittent claudication: multicenter controlled double-blind trial with objective assessment of chronic occlusive arterial disease patients. Am Heart J. 1982;104:66-72.
59. Dawson DL, Cutler BS, Hiatt WR, et al. A comparison of cilostazol and pentoxifylline for treating intermittent claudication. Am J Med. 2000;109:523-530.
60. Girolami B, Bernardi E, Prins MH, et al. Treatment of intermittent claudication with physical training, smoking cessation, pentoxifylline, or nafronyl: a meta-analysis. Arch Intern Med. 1999;159:337-345.
61. Kohda N, Tani T, Nakayama S, et al. Effect of cilostazol, a phosphodiesterase III inhibitor, on experimental thrombosis in the porcine carotid artery. Thromb Res. 1999;96:261- 268.
62. Igawa T, Tani T, Chijiwa J, et al. Potentiation of anti-platelet aggregating activity of cilostazol with vascular endothelial cells. Thromb Res. 1990;57:617-623.
63. Tsuchikane E, Fukuhara A, Kobayashi T, et al. Impact of cilostazol on restenosis after percutaneous coronary balloon angioplasty. Circulation. 1999;100:21-26.
64. Beebe HG, Dawson DL, Cutler BS, et al. A new pharmacological treatment for intermittent claudication: results of a randomized, multicenter trial. Arch Intern Med. 1999;159:2041-2050.
65. Money SR, Herd JA, Isaacsohn JL, et al. Effect of cilostazol on walking distances in patients with intermittent claudication caused by peripheral vascular disease. J Vasc Surg. 1998;27:267-274.
66. Dawson DL, Cutler BS, Meissner MH, Strandness DEJ. Cilostazol has beneficial effects in treatment of intermittent claudication: results from a multicenter, randomized, prospective, double-blind trial. Circulation. 1998;98:678- 686.
67. Brevetti G, Perna S, Sabba C, Martone VD, Condorelli M. Propionyl-l-carnitine in intermittent claudication: double-blind, placebo-controlled, dose titration, multicenter study. J Am Coll Cardiol. 1995;26:1411-1416.
68. Brevetti G, Diehm C, Lambett D. European multicenter study on propionyl-l-carnitine in intermittent claudication. J Am Coll Cardiol. 1999;34:1618-1624.
69. Brevetti G, Perna S, Sabba C, et al. Effect of propionyl-l-carnitine on quality of life in intermittent claudication. Am J Cardiol. 1997;79:777-780.
70. Lievre M, Morand S, Besse B, et al. Oral beraprost sodium, a prostaglandin I(2) analogue, for intermittent claudication: a double-blind, randomized, multicenter controlled trial. Circulation. 2000;102:426-431.
71. Mannarino E, Pasqualini L, Innocente S, et al. Physical training and antiplatelet treatment in stage II peripheral arterial occlusive disease: alone or combined? Angiology. 1991;42:513-521.
72. Scheffler P, de la Hamette D, Gross J, Mueller H, Schieffer H. Intensive vascular training in stage IIb of peripheral arterial occlusive disease. The additive effects of intravenous prostaglandin E1 or intravenous pentoxifylline during training. Circulation. 1994;90:818-822.
73. Dormandy JA, Murray GD. The fate of the claudicant: a prospective study of 1969 claudicants. Eur J Vasc Surg. 1991;5:131-133.
74. O'Riordain DS, O'Donnell JA. Realistic expectations for the patient with intermittent claudication. Br J Surg. 1991;78:861-863.
75. Wilson SE, Wolf GL, Cross AP. Percutaneous transluminal angioplasty versus operation for peripheral arteriosclerosis. J Vasc Surg. 1989;9:1-8.
76. Dormandy JA, Rutherford RB. Management of peripheral arterial disease (PAD). TASC Working Group. J Vasc Surg. 2000;31:S1-S296.
77. Poulias GE, Doundoulakis N, Prombonas E, et al. Aorto-femoral bypass and determinants of early success and late favourable outcome. Experience with 1000 consecutive cases. J Cardiovasc Surg. 1992;33:664-678.
78. Lorentzen JE, Nielsen OM, Arendrup H, et al. Vascular graft infection: an analysis of sixty-two graft infections in 2411 consecutively implanted synthetic vascular grafts. Surgery. 1985;98:81-86.
79. Veith FJ, Gupta SK, Ascer E, et al. Six-year prospective multicenter randomized comparison of autologous saphenous vein and expanded polytetrafluorethylene grafts in infrainguinal arterial reconstructions. J Vasc Surg. 1986;3:104-114.
80. Dalman RL, Taylor LM. Basic data related to infrainguinal revascularization procedures. Ann Vasc Surg. 1990;4:309- 312.
81. Samson RH, Veith FJ, Janko GS, Gupta SK, Scher LA. A modified classification and approach to the management of infections involving peripheral arterial prosthetic grafts. J Vasc Surg. 1988;8:147-153.
82. Nehler MR, Moneta GL, Edwards JM, et al. Surgery for chronic lower extremity ischemia in patients eighty or more years of age: operative results and assessment of postoperative independence. J Vasc Surg. 1993;18:618-626.
83. Nehler MR, Moneta GL, Yeager RA, et al. Surgical treatment of threatened reversed infrainguinal vein grafts. J Vasc Surg. 1994;20:558-565.
84. Nicoloff AD, Taylor LMJ, McLafferty RB, Moneta GL, Porter JM. Patient recovery after infrainguinal bypass grafting for limb salvage. J Vasc Surg. 1998;27:256-263.
85. Yamanaka M, Kwong PK. The side-to-side flap technique in below-the-knee amputation with long stump. Clin Orthop. 1985;201:75-79.
86. Robinson KP. Long posterior flap amputation in geriatric patients with ischaemic disease. Ann R Coll Surg Engl. 1976;58:440-451.
87. Silverman DG, Roberts A, Reilly CA, et al. Fluorometric quantification of low-dose fluorescein delivery to predict amputation site healing. Surgery. 1987;101:335-341.
88. Tripses D, Pollak EW. Risk factors in healing of below-knee amputation. Appraisal of 64 amputations in patients with vascular disease. Am J Surg. 1981;141:718-720.
89. Kihn RB, Warren R, Beebe GW. The "geriatric" amputee. Ann Surg. 1972;176:305-314.
90. Rigdon EE, Monajjem N, Rhodes RS. Criteria for selective utilization of the intensive care unit following carotid endarterectomy. Ann Vasc Surg. 1997;11:20-27.
91. Gregg RO. Bypass or amputation? Concomitant review of bypass arterial grafting and major amputations. Am J Surg. 1985;149:397-402.
92. Cameron HC. Amputations in the diabetic: outcome and survival. Lancet. 1964;ii:605-607.
93. Rush DS, Huston CC, Bivins BA, Hyde GL. Operative and late mortality rates of above-knee and below-knee amputations. Am Surg. 1981;47:36-39.
94. Whitehouse FW, Jurgensen C, Block MA. The later life of the diabetic amputee: another look at the fate of the second leg. Diabetes. 1968;17:520-521.
95. McDermott MM, Mehta S, Ahn H, Greenland P. Atherosclerotic risk factors are less intensively treated in patients with peripheral arterial disease than in patients with coronary artery disease. J Gen Intern Med. 1997;12:209- 215.
96. Orchard TJ, Strandness DE, Cavanagh PR, et al. Assessment of peripheral vascular disease in diabetes. Report and recommendations of an international workshop. Circulation. 1993;88:819-828.